The emerging severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants of concern (VOC) have impacted children and younger adults more adversely due to the different virulence of the VOCs. COVID-19-related cutaneous complications like urticaria, erythema multiforme, chilblain-like lesions in children, and acute hemorrhagic edema in infants of ages between four and five months have been reported. Furthermore, COVID-19-related symptoms of IgA vasculitis have also been observed.
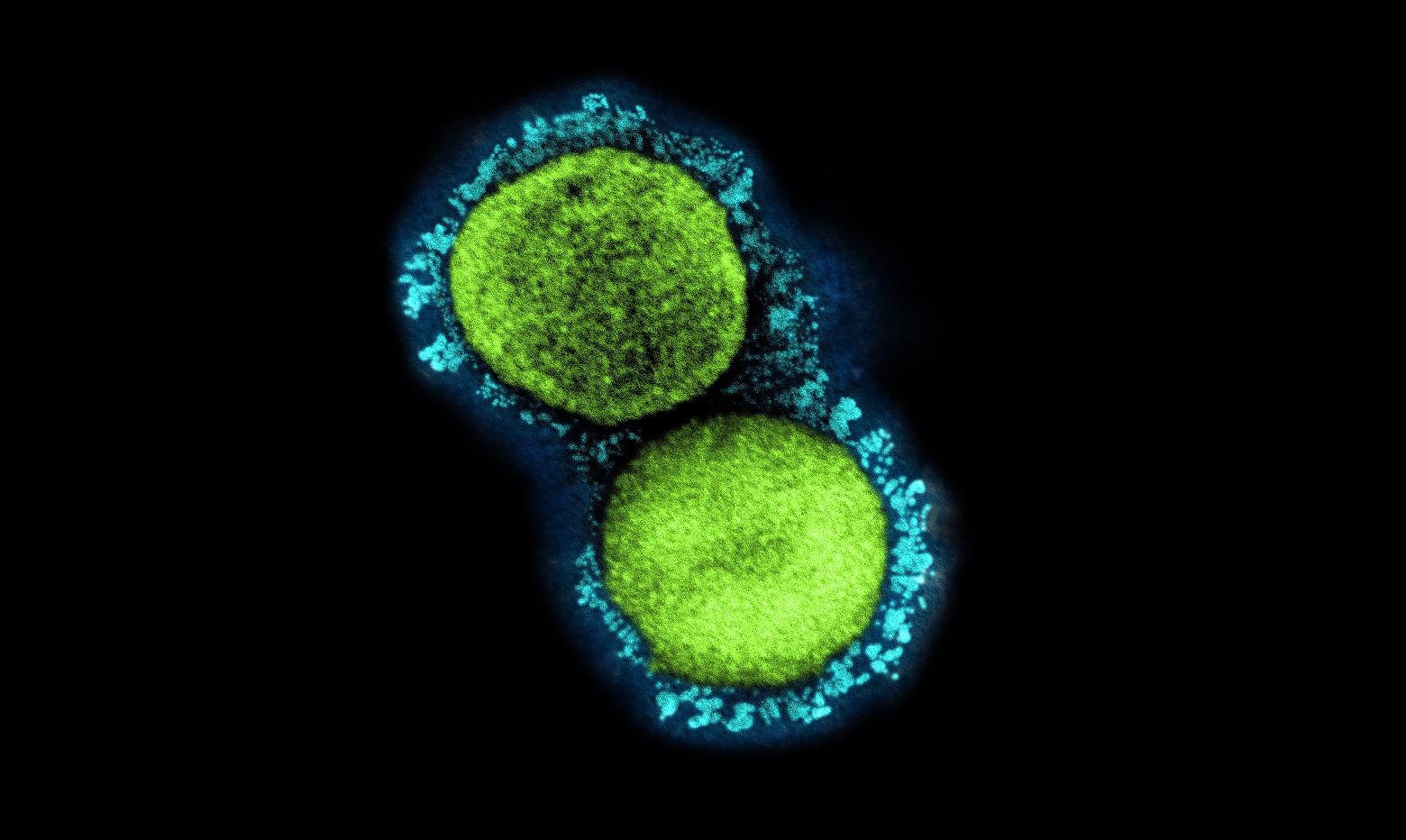 Study: Iga Vasculitis And COVID-19 In Children: A Systematic Review. Image Credit: NIAID
Study: Iga Vasculitis And COVID-19 In Children: A Systematic Review. Image Credit: NIAID

 *Important notice: Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
About the study
The present study reviewed research articles to assess a possible association between COVID-19 infection and IgA vasculitis manifestation in children.
The review included articles published between 1 January 2020 and 30 August 2021 that reported a case of IgA vasculitis associated with COVID-19 or a series of cases with the association. IgA vasculitis cases were selected based on mandatory criteria including palpable purpura without the presence of thrombocytopenia and supportive criteria inclusive of at least one or more manifestations out of acute-onset diffuse abdominal pain, proteinuria, haematuria, or acute-onset arthralgia, arthritis, presence of predominant IgA deposits in proliferative glomerulonephritis, or leukocytoclastic vasculitis. Cases of COVID-19 infection were identified based on SARS-CoV-2 ribonucleic acid (RNA) detection in a sample using a SARS-CoV-2 specific antigen test or a diagnostic molecular amplification test.
The team collected data from each article eligible for the study, including age, gender, comorbidities, symptoms, and the sequential correlation of SARS-CoV-2 detection and IgA vasculitis manifestations.
Causality criteria recommended by the causality assessment system of the World Health Organization-Uppsala Monitoring Center (WHO-UMC) were applied to the selected reports to assess the possible causal association of COVID-19 and IgA vasculitis.
The causality assessment system was used to assess any causal link between the two diseases into one to six different levels of certainty, ranging from certain, probable/likely, possible, unlikely, conditional/unclassified, and unassessable/unclassifiable.
Results
The study results showed that in the 12 eligible reports selected, patients had a mean age of 7.3 years. The 12 patients in each report consisted of three females and nine males. Three had a Mediterranean origin, two were Caucasian, one was Asian, three were Hispanic, one was Black, and two had an unspecified origin. Eight of the 12 patients were reported as healthy, one had unspecified health status, and three had a positive medical history of Hirschsprung disease, atopic dermatitis, and suprasellar germinoma characterized by secondary panhypopituitarism.
As specified in the inclusion criteria, all 12 patients had symptoms of palpable purpura. Furthermore, seven patients had gastrointestinal (GI) symptoms, including two patients who presented hematochezia while abdominal pain was the most common GI manifestation. Oligoarthritis was observed in seven patients, of which five cases presented with ankle pain involvement and one case with one knee involved. Also, three patients had hematuria, while hypertension was not present in any patients. A total of six out of the 12 patients met two of the indicators of IgA vasculitis, six patients met three criteria, and none of the patients met all of the four criteria.
An elevated level of c-reactive protein (CRP) was observed in six patients, while an insignificant number of patients had inflammatory markers like ferritin and D-dimer. Out of the 12 patients, four presented elevated IgA levels. One had normal IgA levels, while the IgA levels of seven patients were not measured.
In 83% of the cases, SARS-CoV-2 was detected after the presentation of IgA vasculitis symptoms or after the patient sought medical attention. In two or 17% of the total patients, a COVID-19-positive diagnosis was observed before the presentation of IgA vasculitis. One of these patients was tested COVID-19-positive two days before the appearance of IgA vasculitis symptoms, while the other patient was detected COVID-19-positive 37 days prior to symptom onset.
Conclusion
The study findings showed that the 12 identified cases provided sufficient evidence of association of IgA vasculitis with or without the presence of SARS-CoV-2 infection in children.
A prevalence of COVID-19-related IgA vasculitis was noted, particularly in early childhood. Furthermore, the increase in association of COVID-19 and IgA vasculitis was observed thrice as many times in males than in females, while non-COVID-19-associated IgA vasculitis was detected five times more in males than females.
The inflammatory responses of COVID-19 are very similar to the manifestations of autoimmunity. Although the exact role of SARS-CoV-2 in the manifestation of IgA vasculitis is still unknown, further research to investigate the specific association can help manage the two conditions more efficiently.

 *Important notice: Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.