Infectious disease outbreaks, such as COVID-19, adversely impacted public health and had socioeconomic consequences. Research shows that deploying effective public health strategies, such as a “Find, Test, Trace, Isolate” (FTTI) strategy that identifies and quarantines infectious individuals to prevent onward transmission could help minimize the harm caused by pandemics.
During the COVID-19 pandemic, FTTI systems reliant on lab-based tests, such as reverse transcriptase-polymerase chain reaction (RT-PCR), failed to mitigate onward severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission. Notably, RT-PCR tests have a long turnaround time and cannot detect presymptomatic and asymptomatic SARS-CoV-2-infected individuals (forming a hidden infection chain).
Digital contact tracing techniques, such as wearable sensors, have the potential to fill these gaps and detect infections caused by respiratory pathogens, including SARS-CoV-2, before the onset of symptoms or even in the absence of symptoms. Wearable sensors also offer the benefit of passive monitoring, which minimizes the need for user engagement, and preserves user privacy (not shared with a centralized database).
As they offer several potential benefits, several studies have focused on developing wearable sensor-based infectious disease detection algorithms; however, none have explored the impact of deploying these devices for pandemic mitigation in a real-world setting.
About the study
In the present study, researchers built a compartmental epidemiological model based on a Susceptible, Exposed, Infectious, Removed (SEIR) framework in which wearable devices notified users of potential SARS-CoV-2 infection and prompted them to seek a lab-based test and self-isolate while awaiting the result.
The study simulated the wearable sensor deployment scenarios during Canada’s second COVID-19 pandemic wave from September 1, 2020, to February 20, 2021. First, the researchers considered a baseline scenario where wearable device users could download an application with currently available detection algorithms. Next, they investigated the impact of technology and behavioral parameters, such as detection accuracy, sensitivity, specificity, uptake (defined as users using wearables often), and adherence (defined as users who take the appropriate next steps after a positive notification of SARS-CoV-2 infection). Additionally, the researchers tested a complementary approach using rapid antigen tests (RATs) to confirm SARS-CoV-2 infection notified by wearables.
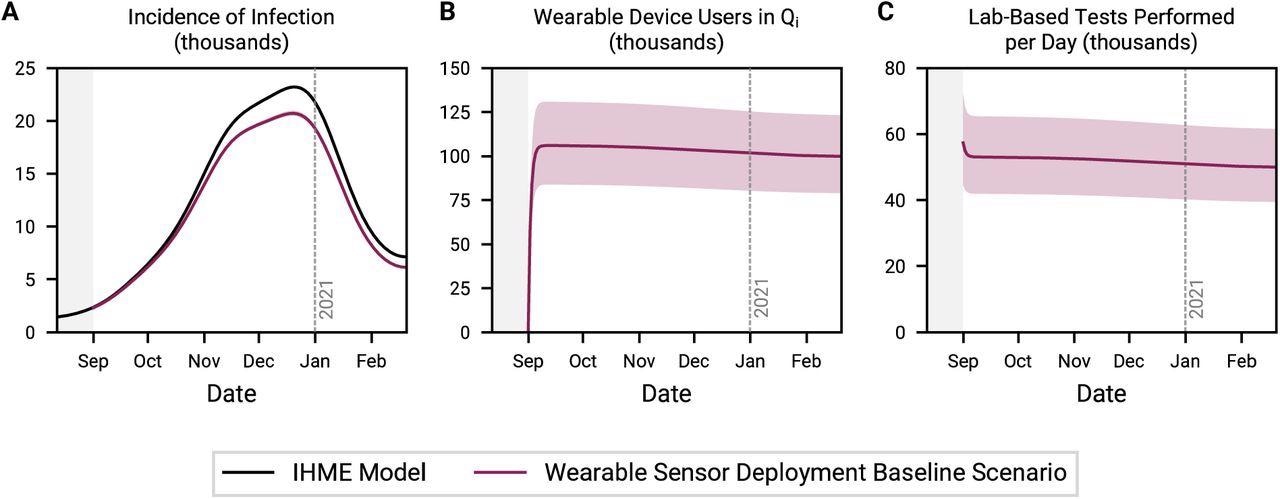
Baseline scenario for wearable sensor deployment. Time series depiction of the incidence of infection (A), the number of wearable device users incorrectly in quarantine (B), and the daily demand for lab-based tests (C). Uptake, adherence, detection sensitivity, and detection specificity are set to 4%, 50%, 80%, and 92%, respectively.
Study findings
The present study has several significant findings. First, although wearable sensor deployment reduced the burden of infection by decreasing the pool of infectious individuals, it depended largely on detection algorithm specificity. Low detection specificity results in false-positive notification of potential SARS-CoV-2 infection leading to unnecessary quarantines, thereby decreasing the pool of susceptible individuals.
Without improvements to detection specificity, every user would spend an average of two more days a month unnecessarily quarantining, and close to 40,000 to 65,000 additional lab-based tests per day would be required. In addition, the associated social and economic harm would likely undermine public confidence in and compliance with a wearable-based pandemic mitigation strategy. Therefore, along with prioritizing uptake and adherence of wearables, their associated cost should be accounted for before deployment.
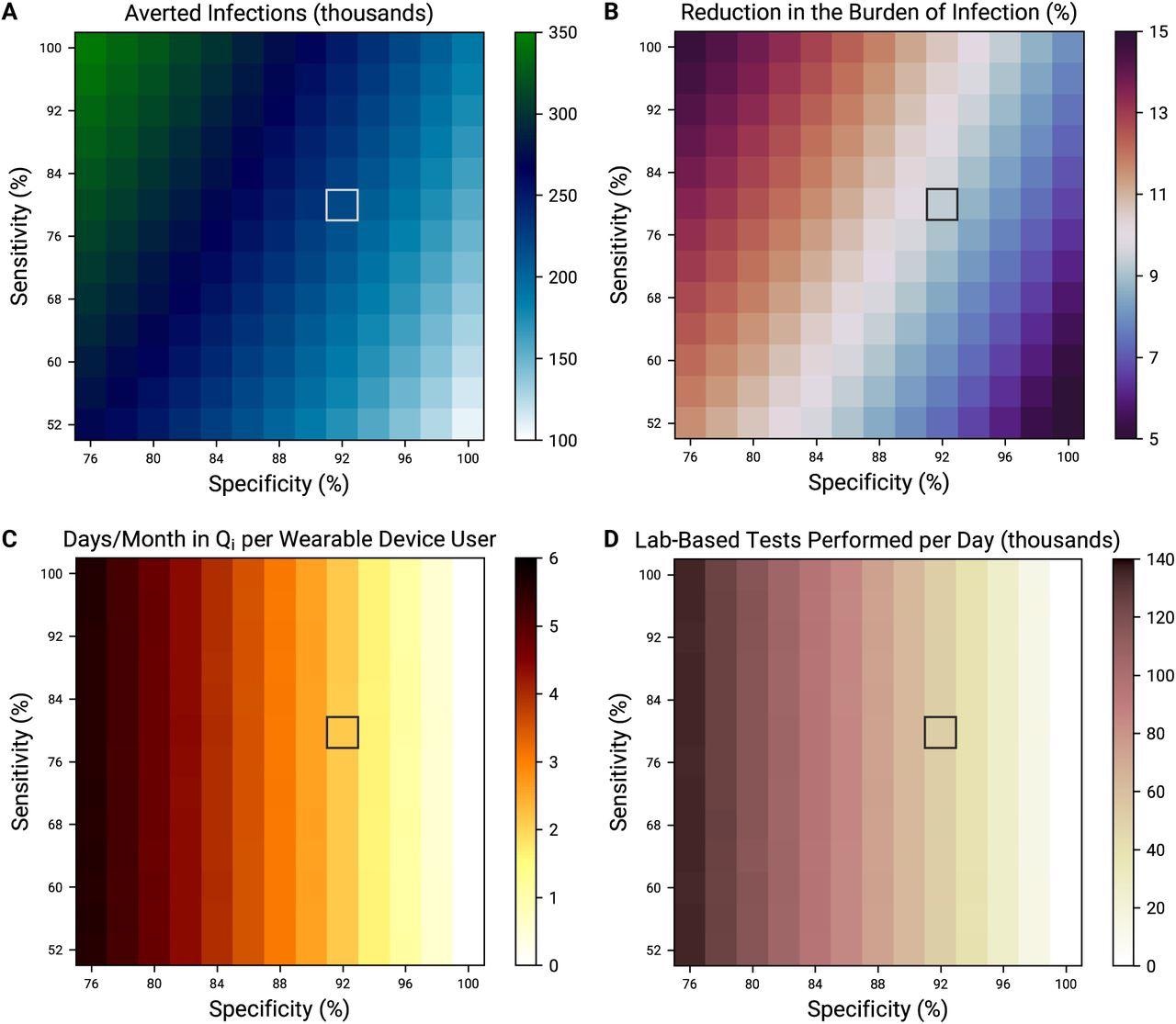
Tradeoff between detection sensitivity and specificity. Averted infections (A), reduction in the burden of infection (B), days incorrectly spent in quarantine per month per device user (C), and average daily demand for lab-based tests (D), all over the entire simulation period, as a function of detection sensitivity and specificity. Grey boxes denote nominal sensitivity (80%) and specificity (92%).
Another effective solution would be the inclusion of confirmatory antigen testing to increase the overall specificity of the strategy and decrease the overall false-positive rate. Introducing RATs would reduce days spent in quarantine by ~300-fold, simultaneously bringing down the additional demand on lab-based testing infrastructure to moderate levels. However, this would not 100% compensate for poor detection specificity.
With higher detection specificity, the authors noted a four-fold reduction in quarantining days per month per user (incorrectly spent by user). They also observed a two-fold reduction in lab-based tests performed each day and a five-fold reduction in antigen tests used each day.
Overall, wearable deployment is more advantageous than broad antigen test-based screening approaches that require high manufacturing volumes, infrastructure, and funding; wearables non-invasively detect SARS-CoV-2 infections without active user engagement.
Conclusions
According to the authors, this is the first study that explored wearable sensor deployment scenarios as a COVID-19 mitigation strategy. The use of wearables would enable real-time detection of presymptomatic and asymptomatic SARS-CoV-2 infections. By complementing and supporting FTTI systems, their deployment would also reduce the burden of SARS-CoV-2 infections and help mitigate the pandemic.
However, in scenarios where detection algorithm specificity was low, complementary interventions, such as RATs, potentially reduced false positives, thereby minimizing costs and reducing the burden on resources.
Future studies should explore better ways to incorporate wearable sensors into FTTI systems for pandemic mitigation; and identify how these devices could continue to be used for public health benefits, complementary to vaccines, to inform future research investment and policy.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Deploying wearable sensors for pandemic mitigation, Nathan Duarte, Rahul Arora, Graham Bennett, Meng Wang, Michael P Snyder, Jeremy R Cooperstock, Caroline E Wagner, medRxiv 2022.02.07.22270634; doi: https://doi.org/10.1101/2022.02.07.22270634, https://www.medrxiv.org/content/10.1101/2022.02.07.22270634v2
- Peer reviewed and published scientific report.
Duarte, Nathan, Rahul K. Arora, Graham Bennett, Meng Wang, Michael P. Snyder, Jeremy R. Cooperstock, and Caroline E. Wagner. 2022. “Deploying Wearable Sensors for Pandemic Mitigation: A Counterfactual Modelling Study of Canada’s Second COVID-19 Wave.” Edited by Danilo Pani. PLOS Digital Health 1 (9): e0000100. https://doi.org/10.1371/journal.pdig.0000100. https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0000100.