While speaking, sneezing, coughing, singing, laughing, and breathing out, humans exhale particles containing respiratory fluids. Sometimes these exhaled particles may also contain infectious pathogens.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Background
Typically, the diameter of the exhaled particles is between 0.01 and 1,000 micrometers (µm). These particles can be classified as those with a diameter smaller than 5 µm, which are referred to as droplet nuclei or aerosols, or those with a diameter larger than 5 µm in diameter that is known as respiratory droplets. The size of the exhaled particles changes continually based on the environment, especially due to evaporation.
The size of the exhaled particles influences the transmission modes of airborne particles. Apart from size, the transmission of particles also depends on ventilation and airflow. It is important to distinguish aerosols and droplets, as their size effectively separates their aerodynamic behavior, ability to be inhaled, and efficacy of interventions.
Modeling to predict the fate of exhaled particles
Scientists have developed several models to predict the fate of exhaled particles in different environments. These models, which have varied complexities and resolutions for determining fluid flow and dispersion, provide information on aerosol and droplet dynamics including the evaporation, setting, and transportation of exhaled particles in the environment.
A large number of studies related to the generation of droplets and aerosols through violent exhalation like coughing and sneezing are currently available. It is important to correlate coughing with the transmission of the virus.
To date, researchers have documented that viral load is the main driver of transmission. The evolution of modeling approaches has enabled the assessment of different physical processes associated with exhaled particles.
A rapid advancement related to the modeling of these particles in different environments has been made, which is important to understand the mode of disease transmission. These models must be validated by comparing them with each other through the use of a common set of input parameters. This would ensure that model differences can be deduced in terms of model physics, rather than unspecified differences in model input parameters.
About the study
A new study published on the medRxiv* preprint server generated a consolidated set of parameters involving the exhalation of particles. These parameters could serve as a benchmark for many modeling approaches. In this study, researchers have primarily focused on defining parameters for breathing and speaking.
Herein, the researchers stated that breathing could be modeled as an unsteady phenomenon or simplistically modeled as a constant flow rate, for which a set of self-consistent parameters were applied to both approaches.
To this end, a differential rate of flow velocities at the mouth or nose opening and exhalation only occurs for approximately half of the breathing period. Some of the parameters associated with exhalation include the area of the opening, projection angle, density, environmental condition including temperature and relative humidity, average flow rate, and exhaled particle composition, such as whether sodium chloride or proteins, for example, are present within the droplets.
Study findings
When the exhaled air flow rate was modeled as a steady flow, the average flow rate was obtained by dividing the total exhaled volume by the breathing period. The authors estimated an average exhalation flow rate of 10.6 L min-1 for an average male and 8.3 L min−1 for an average female. These values are related to the exhalation flow rate while breathing.
A previous study proposed that the BLO model could be applied to analyze the size distribution of particles in different locations of the airways, which can include bronchiolar (B), laryngeal (L), and oral (O). Moreover, another study found that patients hospitalized with coronavirus disease 2019 (COVID-19) exhale respiratory particles (aerosols) whose sizes are similar to those from a healthy individual while breathing, speaking, and coughing.
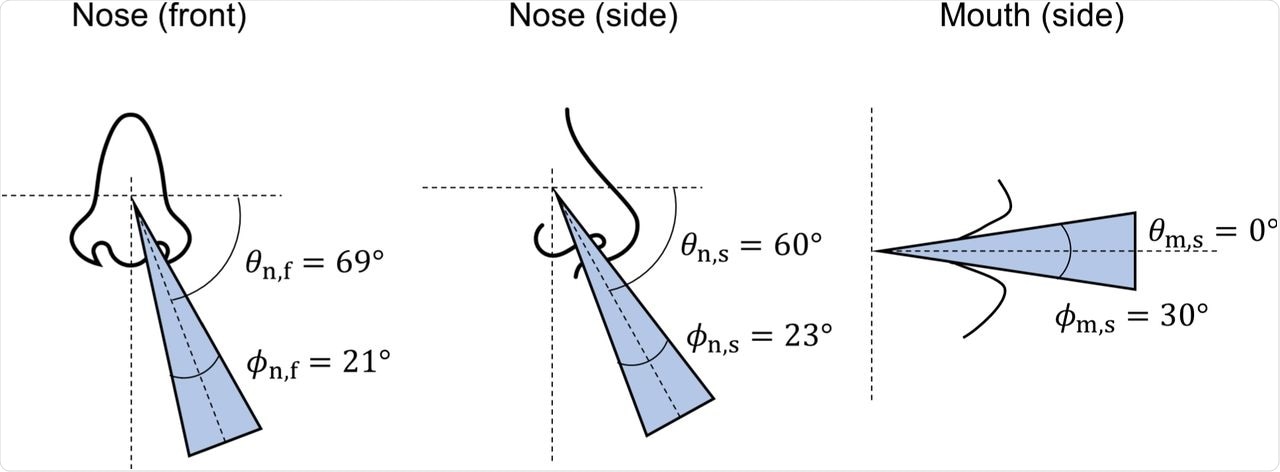
Graphical representation of jet projection (θ) and spreading (ϕ) angles.
Although previous studies have also detected the presence of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), the causal agent of COVID-19, in exhaled breath condensate (EBC) of an infected person, there remains a gap in research regarding the viral load in different particle sizes. Thus, the authors did not include concentrations of pathogens in the set of parameters for exhaled particles.
Conclusions
The current study defined a set of parameters that could be used as a benchmark of modeling studies associated with variabilities in particles exhaled by an individual in terms of their volume, composition, size, velocity rate, density, and viral load.
The authors highlighted the unavailability of evidence to quantify the modal, mean, or median parameter values within the population. Moreover, they emphasized that modeling the fate of exhaled particles when performed with valid parameters could elucidate the possible transmission pathways and, as a result, assist in the development of preventive strategies.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Stettler, J. E. M., Nishida, R. T., de Oliveira, P. M., et al. (2022) Source terms for benchmarking models of SARS-CoV-2 transmission via aerosols and droplets. medRxiv. doi:10.1101/2022.02.11.22270844. https://www.medrxiv.org/content/10.1101/2022.02.11.22270844v1.
- Peer reviewed and published scientific report.
Stettler, Marc E. J., Robert T. Nishida, Pedro M. de Oliveira, Léo C. C. Mesquita, Tyler J. Johnson, Edwin R. Galea, Angus Grandison, et al. 2022. “Source Terms for Benchmarking Models of SARS-CoV-2 Transmission via Aerosols and Droplets.” Royal Society Open Science 9 (5). https://doi.org/10.1098/rsos.212022. https://royalsocietypublishing.org/doi/10.1098/rsos.212022.