Dysregulation of hemostasis could lead to bleeding or thrombotic complications, which are often caused by a hypercoagulable state. This state is also observed in coronavirus disease 2019 (COVID-19) patients. COVID-19 is caused by a novel coronavirus, namely, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Thrombotic events are common among COVID-19 patients requiring hospitalization, and such events could not be predicted using routine coagulation assays. In this regard, ROtational ThromboElastoMetry (ROTEM) has been proposed as a promising tool by many recent studies.
A new study published in the journal Diagnostics provided an overview of ROTEM with a particular focus on interpreting the symmetrical clot formation curve. Researchers also introduced new parameters that could aid in distinguishing between COVID-19 patients and outcomes.
Study: The Composition and Physical Properties of Clots in COVID-19 Pathology. Image Credit: donfiore / Shutterstock
ROTEM and Interpretation
Standard hemostasis assays neglect the complex interaction between coagulation proteases, platelets, and other cells. Assays, such as the prothrombin time (PT) or activated partial thromboplastin time (aPTT), heavily depend on the first fibrin fibers to be formed and detected. These are mainly suited to identify the presence of anticoagulants or deficiencies. However, they are not used for hypercoagulability or thrombosis risk estimation. The gold standard is of course, the light transmission aggregometry (LTA), whereby platelets block light signals in the plasma, but even LTA is not sensitive enough for evaluating platelet hyperreactivity.
Laboratory methods have been developed to incorporate the almost complete coagulation cascade, and two main methods in this domain are ThromboElastoGraphy (TEG) and ROtational ThromboElastoMetry (ROTEM), where a pin is suspended in a cup with whole blood. In ROTEM, the cup is fixed with a rotating pin, while the reverse occurs in TEG. As the blood forms a platelet-rich fibrin thrombus (clotting), the rotation is hindered, and the degree of hindrance is recorded as amplitude (A) and expressed in mm against time. The outcome is a symmetric-looking graph, and the magnitude of this reaction curve is proportional to the strength of the clot formed over time. This enables the characterization of the clot formation.
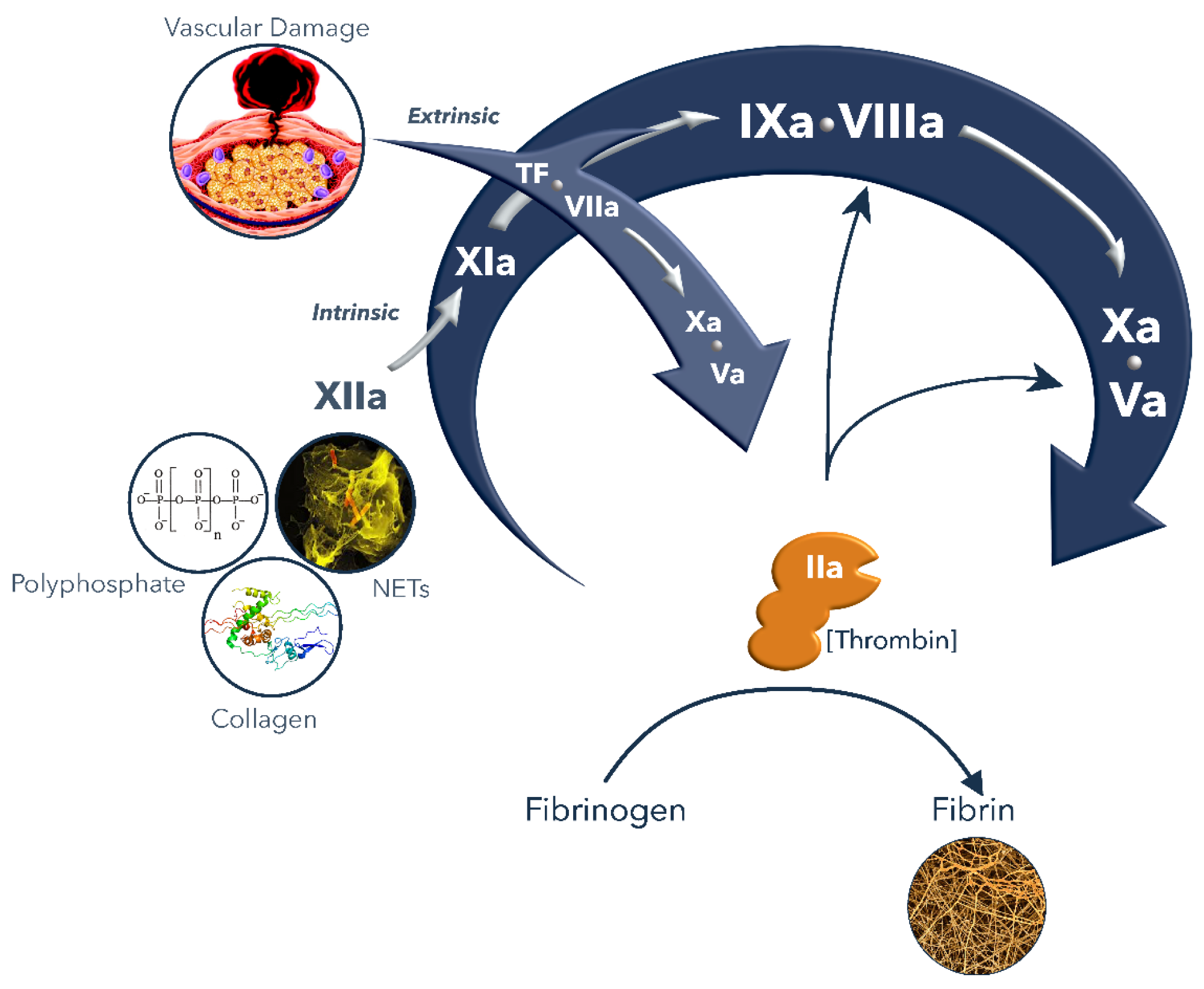 Highlight of the coagulation cascade
Highlight of the coagulation cascade
Coagulopathy in COVID-19 and Novel Parameters from ROTEM
Standard assays cannot identify COVID-19 patients at risk of thrombotic complications, and about 25% of patients in intensive care suffer from such events. COVID-19 induced coagulopathy has displayed very unique clinical phenotypes, and biochemical properties and cases of thromboembolism have been observed despite administering anticoagulant medication.
COVID-19 coagulopathy also entails increased levels of fibrinogen and markers of endothelial activation. Further clinical studies are required to analyze the effect of combined pathologies on hypercoagulability and outcomes in global assays such as ROTEM.
More specifically, this seems a feasible technology to study the fibrin formation and lysis in COVID-19 patients. As predictors of thromboembolic complications, three key ROTEM variables have been studied. These are the MCF (maximum clot firmness), CT (clotting time), and CFT (clot formation time). An explosive generation of fibrin with a strongly elevated MCF are the characteristics of a ROTEM of a COVID-19 patient, as opposed to a healthy individual. Additionally, no lysis is detectable in the COVID-19 samples.
The ROTEM parameters cannot describe all aspects of the differences (e.g., rate of clot formation) between a healthy person and a COVID-19 patient. To gain better insight into clot formation, researchers re-analyzed the ROTEM data reported in a previous study to introduce two novel parameters - Clot Firmness Increase (CFI) and Slope-MCF-t (in mm/min). They compared the slope-CFT and slope-MCF-t in whole blood samples with and without additional spiking of fibrinogen and/or heparins. Scientists observed that both the parameters were significantly higher upon fibrinogen spiking. However, the elevated values did not change upon the addition of heparin.
Besides COVID-19, hypercoagulability has been long associated with several other cardiovascular and non-cardiovascular pathologies, such as malignancies. ROTEM can identify hypercoagulable states in patients suffering from a wide range of conditions and has shown a promising precision for monitoring thromboprophylaxis in patients receiving LMWH and DOACs and in vitro.
Concluding Remarks
Thrombotic complications in COVID-19 are unpredictable in terms of occurrence and severity. ROTEM has been shown to be a promising alternative to conventional coagulation assays, such as PT and aPTT. To treat hypercoagulability and hyperfibrinolysis in COVID-19 patients, further research on clot formation in COVID-19 samples could be beneficial. Novel parameters, such as the CFI and Slope-MCF-t might provide deeper insights into the rate of clot formation. Researchers, however, stated that further validation of these novel parameters is required to illustrate and establish their importance.