Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) via its mutant variants tend to escalate the COVID-19-related mortality and morbidity across the world. Infection prevention and control strategies combined with mass COVID-19 vaccination is an efficient approach to limit and halt the ongoing SARS-CoV-2 pandemic. Yet, it is critical to uncover factors that influence vaccine effectiveness parallel to continuing to expand immunization efforts. SARS-CoV-2 vaccinations efficacy in non-immunocompromised persons in the United States (US) has been established. Nonetheless, the effect of chronic health conditions (CHC) on the serostatus following COVID-19 vaccination remains uncertain.
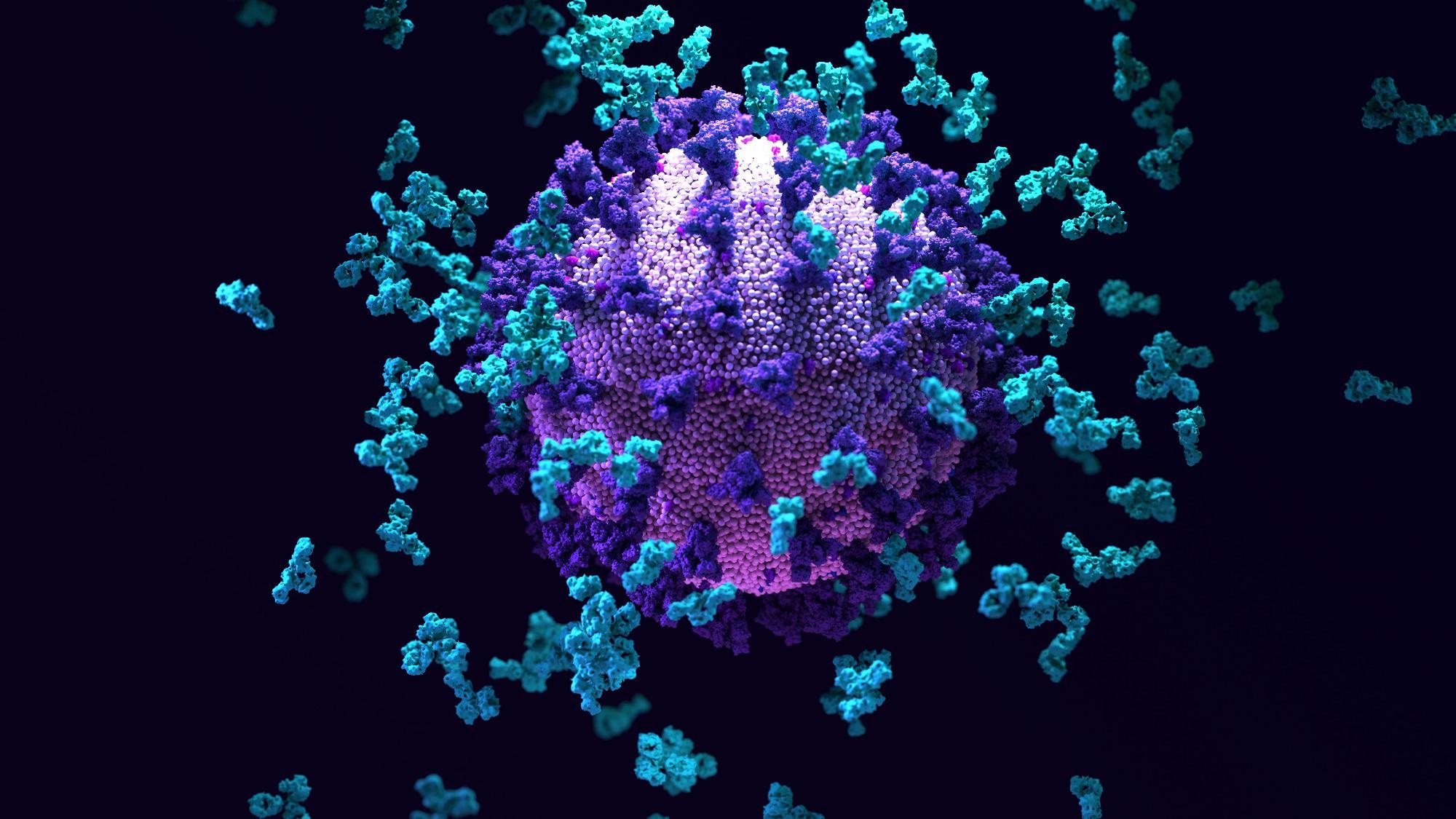 Study: Comorbidities Diminish the Likelihood of Seropositivity After SARS-CoV-2 Vaccination. Image Credit: Design_Cells / Shutterstock
Study: Comorbidities Diminish the Likelihood of Seropositivity After SARS-CoV-2 Vaccination. Image Credit: Design_Cells / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
About the study
In the current study, the researchers examined the impact of comorbidities on the serostatus after SARS-CoV-2 vaccination. The data for the present study were gathered from the Co-Immunity Project, federally-sponsored ongoing population-based research in Jefferson County, Kentucky, United States of America (USA), to monitor SARS-CoV-2.
Adults aged 18 years or older who were fully vaccinated against COVID-19 and resided in Jefferson County, Kentucky, were enrolled for the present study between April and August 2021. This study was performed during the start of the SARS-CoV-2 Delta wave in the US. According to the Centers for Disease Control and Prevention (CDC), subjects were deemed "fully vaccinated" if their last vaccine shot (i.e., second dose for Pfizer-BioNTech or Moderna and first dose for Janssen) was more than 14 days before the study visit. This study's subjects were all within nine months of receiving their final vaccine dose. The participants were recruited after submitting a signed informed consent.
The study subjects self-documented their health history, including pre-existing CHC and medicines. Lupus, rheumatoid arthritis, and other autoimmune diseases were grouped under a single variable called "autoimmune diseases." Steroids, baricitinib, and other immune suppressant drugs were merged into a single variable called "immunosuppressants." All cancer treatment approaches, such as chemotherapy, surgery, and immunotherapy, were merged into a single variable called "cancer treatment." Angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) usage was integrated into a single variable called "ACEI or ARB."
Blood finger-prick and nasopharyngeal swab samples were taken by trained personnel. The reverse transcription-polymerase chain reaction (RT-PCR) was used to check for SARS-CoV-2 infection in the samples. COVID-19 serostatus was assessed by measuring SARS-CoV-2 spike (S) protein-specific immunoglobulin G (IgG) antibodies in peripheral blood samples using an enzyme-linked immunoassay (ELISA).
Results
The results showed that of the 7,046 subjects recruited, 1,868 individuals were removed from the analysis since 802 were unvaccinated, 487 lacked vaccination dates or other essential vaccine-associated information, 247 lacked medical history or relevant demographic data, and 332 did not have a fully vaccinated status. Further, among the eligible 5,178 COVID-19 fully vaccinated subjects, 5,127 were SARS-CoV-2 seropositive, whereas 51 were seronegative.
Autoimmune disease and chronic kidney disease (CKD) demonstrated the highest connections to SARS-CoV-2-negative serostatus in the fully vaccinated subjects. The lack of any CHC was closely linked to SARS-CoV-2 seropositivity. The chance of SARS-CoV-2-negative serostatus rose as the number of co-existing CHCs increased. Similarly, the use of two or more CHC-associated drugs substantially correlated with seronegative status.
In detail, while 42% of those with no-CHC were SARS-CoV-2 seropositive, 22% had negative serostatus. In people with CKD, 2% had a seropositive status, whereas 12% were SARS-CoV-2 seronegative. Further, 31% among the autoimmune disease category were seronegative, whereas 5% had positive serostatus. Seronegative status was also considerably high in patients with hypertension, cardiovascular diseases (CVDs), and diabetes.
In addition, 78% of the patients in the seronegative category had any of the CHCs, while 58% of the seropositive lot had at least one CHCs. The seronegative group also had a higher history of cancer therapies and immunosuppressants. By contrast, the history of ACEI or ARB did not correlate with serostatus.
Seronegative status was not significantly linked with age above 65 years, gender, or a documented history of tobacco product use. The existence of even one reported CHC, on the other hand, was strongly linked to SARS-CoV-2 seronegative status. Likewise, when the number of CHCs increased from two to three or more, the pre-existing CHCs correlation with the seronegative status became stronger.
Conclusions
The study findings demonstrated that people who were fully vaccinated against SAR-CoV-2 were more likely to be seronegative if they had any CHC, notably autoimmune illness or CKD. This risk rose as the number of comorbidities increased, particularly while using multiple drugs. The lack of any CHC was protective, increasing the chances of positive serological response after COVID-19 immunization. More research is needed to see if smoking and other comorbid conditions affect the efficiency of the viral neutralization abilities after SARS-CoV-2 immunization.
Overall, the current study implied that almost 50% of the US adults with concurrent CHCs have twice the risk of COVID-19 or reinfection, regardless of a fully vaccinated status compared to those who did not have CHCs. Although CVD, diabetes, and hypertension are established risk factors for severe SARS-CoV-2 outcomes, the present research demonstrated that CKD is a significant threat for COVID-19 vaccination failure. These findings will aid in the development of appropriate COVID-19 vaccination booster doses, targeted vaccination rollout, and identify people with a higher chance of breakthrough SARS-CoV-2 infection globally.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Comorbidities Diminish the Likelihood of Seropositivity After SARS-CoV-2 Vaccination, Alok R. Amraotkar, Adrienne M. Bushau-Sprinkle, Rachel J. Keith, Krystal T. Hamorsky, Kenneth R. Palmer, Hong Gao, Shesh N. Rai, Aruni Bhatnagar. medRxiv 2022.03.15.22272432; DOI: https://doi.org/10.1101/2022.03.15.22272432, https://www.medrxiv.org/content/10.1101/2022.03.15.22272432v1
- Peer reviewed and published scientific report.
Amraotkar, Alok R., Adrienne M. Bushau-Sprinkle, Rachel J. Keith, Krystal T. Hamorsky, Kenneth E. Palmer, Hong Gao, Shesh N. Rai, and Aruni Bhatnagar. 2022. “Pre-Existing Comorbidities Diminish the Likelihood of Seropositivity after SARS-CoV-2 Vaccination.” Vaccines 10 (8): 1363. https://doi.org/10.3390/vaccines10081363. https://www.mdpi.com/2076-393X/10/8/1363.