The ongoing pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has a high mortality rate, with acute respiratory distress syndrome (ARDS) with pneumonia being the most severe manifestation of the disease. The coronavirus disease 2019 (COVID-19) has also been associated with an increased risk of several cardiovascular complications including stroke and myocardial infarction.
However, studies correlating the incidence of thromboembolism with SARS-CoV-2 infection show contradictory results. Meanwhile, thromboprophylaxis may also precipitate bleeding complications.
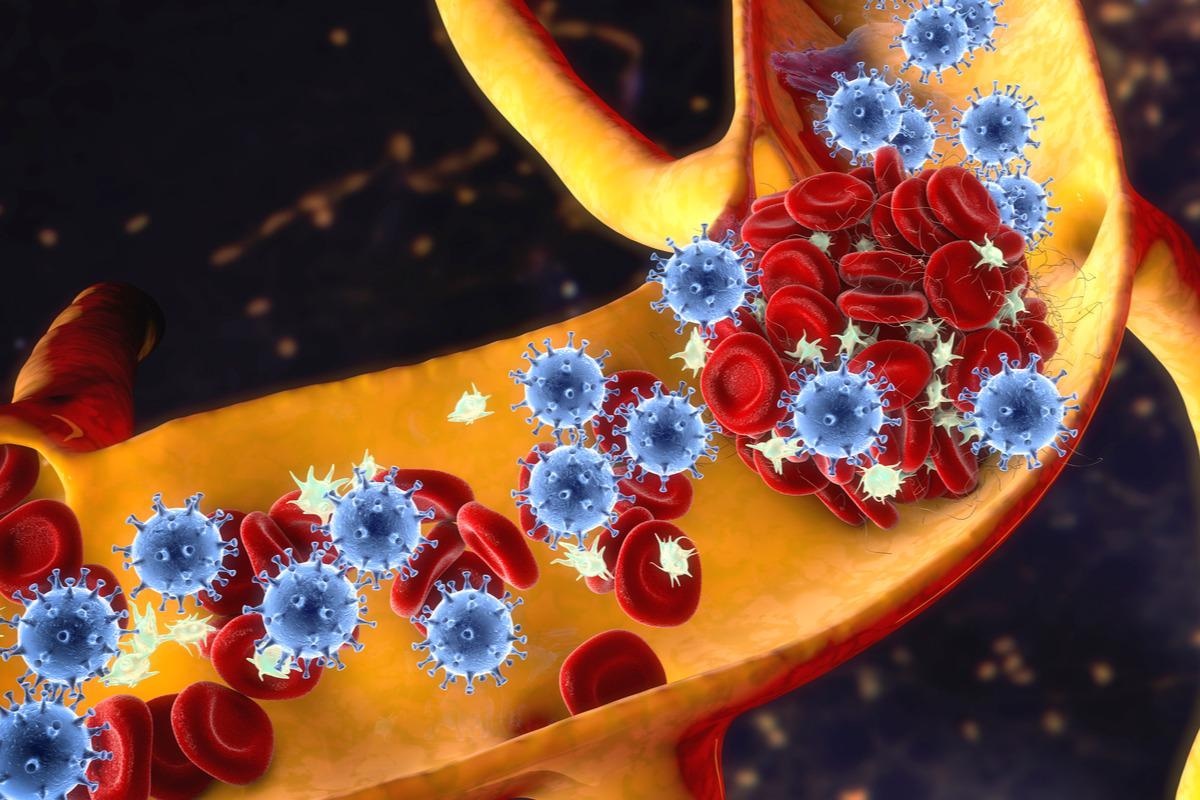
Study: Risks of deep vein thrombosis, pulmonary embolism, and bleeding after covid-19: nationwide self-controlled case series and matched cohort study. Image Credit: Kateryna Kon / Shutterstock.com
About the study
In a recent British Medical Journal study, researchers assess the risk of pulmonary embolism (PE), deep vein thrombosis (DVT), and bleeding among people who have recovered from COVID-19, regardless of their disease severity. The current study was conducted in Sweden between February 1, 2020, and May 25, 2020, and consisted of a matched cohort and self-controlled case series methodologies.
COVID-19 and DVT
Here, 1,057,174 SARS-CoV-2 positive patients with a mean age of 40.2 years were matched to 4,076,342 controls based on gender, age, and country.
During the study period of the case-controlled case series, 1,761 participants experienced their first DVT. As compared to the control period, the incidence rate ratio of this event increased gradually until the second week post-COVID-19 and then increased significantly until day 70.
In addition, a significantly increased incidence rate ratio was also noted in the pre-COVID-19 days -3 to 0 before exposure and 30 days pre-SARS-CoV-2 infection.
The incidence rate ratio during days one through 90, post-COVID-19 increased with age and was the highest during the first wave of the pandemic. Notably, no correlation was found between DVT and COVID-19 with respect to the participants’ gender. A higher risk of DVT was associated with severe SARS-CoV-2 infections.
In the matched cohort study, the first DVT occurred in 267 controls and 401 COVID-19 patients during the 30-days follow-up period. The risk ratio of this event up to 30 days post-COVID-19 was comparable to the incidence rate ratio in the case-controlled case series.
Moreover, the risk ratio increased with severe SARS-CoV-2 infection and was higher during the first wave of COVID-19. All DVT events between one and 30 days post-COVID-19 or the index date occurred in 594 COVID-19 patients and 579 control group participants. The adjusted risk ratio was 4.5 post-COVID-19 for all events of DVT.
All results remained significant after adjusting for the consequences of cancer diagnosis, comorbidities, long-term anticoagulation therapy, and surgery. Notably, long-term anticoagulation therapies did not confer any protection against DVT.
COVID-19 and PE
During the study period of the case-controlled case series, 3,267 participants experienced their first PE. As compared to the control period, the incidence rate ratio of this event increased gradually until the second week post-COVID-19 and then increased significantly until day 110. A significant increase in the incidence rate ratio was also recorded in the pre-COVID-19 days before exposure and 30 days pre-SARS-CoV-2 infection.
The pandemic, together with the sex and age of the participants, significantly affected the event. The incidence rate ratio was higher in males and highest among individuals in the age-range 50-70 years and during the first two weeks post-COVID-19 in the first wave of the pandemic.
However, the incidence rate ratio post-acute phase of SARS-CoV-2 infection was higher during the third wave of the pandemic. Severe SARS-CoV-2 infection was associated with an increased risk of PE.
During days 1-30 post-COVID-19 or the index date PE occurred among 171 in the control group and in 1,761 COVID-19 patients. The risk ratio for first-time PE during the first month post-COVID-19 was comparable to the incidence rate ratio
A higher risk of PE was associated with severe SARS-CoV-2 infections, which was substantially high in hospitalized or intensive care unit (ICU)-admitted patients. The risk of disease was highest during the first wave of the pandemic.
For all the events in the matched cohort study, 2,226 cases of PE were reported in COVID-19 patients and 444 cases in control group participants. All results remained significant after adjusting for the consequences of cancer diagnosis, comorbidities, long-term anticoagulation therapy, and surgery. Notably, long-term anticoagulation therapies conferred protection against PE.
COVID-19 and bleeding events
During the study period of the case-controlled case series, 7,927 participants experienced their first bleeding event. As compared to the control period, the incidence rate ratio of this event decreased gradually until the second week post-COVID-19 and then increased significantly until day 60.
A significant increase in the incidence rate ratio was also observed in the pre-SARS-CoV-2 exposure days before exposure and 30 days pre-COVID-19. The pandemic, together with the sex and age of the participants, significantly affected the modifiers.
The incidence rate ratio was higher among males during the initial two months post-COVID-19 and increased with the age of the patients and was highest during the first wave of the pandemic. Severe SARS-CoV-2 infection was associated with an increased risk of bleeding, whereas no risk was found in mild cases.
During days one through 30 post-COVID-19 or the index date, the first bleeding event occurred in 1,292 control group participants and 1,002 COVID-19 patients. The risk ratio for first-time bleeding was comparable to the incidence rate ratio considering the same period.
A higher risk of PE was associated with severe SARS-CoV-2 infections; however, no increase was seen in mild COVID-19 patients. All events of bleeding in the matched cohort study between one and 30 days post-COVID-19 or the index date occurred in 1,677 COVID-19 patients and 2,370 control group participants.
All results remained significant after adjusting for the consequences of cancer diagnosis, comorbidities, long-term anticoagulation therapy, and surgery. Long-term anticoagulation therapies were associated with increased bleeding risk.
Conclusions
The study findings indicate that SARS-CoV-2 infection is a risk factor for PE, bleeding, and DVT. The association between COVID-19 and these conditions should be considered before prescribing any drug against venous thromboembolism.
Journal reference:
- Katsoularis, I., Farrington, P., Haggstrom, E., et al. (2022). Risks of deep vein thrombosis, pulmonary embolism, and bleeding after covid-19: nationwide self-controlled case series and matched cohort study. BMJ. doi:10.1136/bmj-2021-069590