In a recent study under consideration at Nature Portfolio Journal and posted to the Research Square* preprint server, researchers characterized severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike (S)-specific cluster of differentiation 8 (CD8+) T cell responses.
Understanding the T-cell responses which potentially prevent progression to severe coronavirus disease 2019 (COVID-19) is crucial for developing novel vaccination strategies. In addition, improving future vaccine efficacy against SARS-CoV-2 variants of concern (VOCs) is crucial. In fact, COVID-19 vaccines should induce CD8+ T cells with polyfunctional cytotoxicity and cross-reactivity towards SARS-CoV-2 VOCs, including Delta and Omicron.
Cytotoxic CD8+ T cells are a critical component of vaccine-induced protective immunity. They suppress symptom severity, and studies have shown that their depletion is associated with a poor prognosis in COVID-19 patients. Moreover, CD8+ T-cell responses, generally induced after the second dose of messenger ribonucleic acid (mRNA) vaccines, such as mRNA-1273 and BNT162b, persists for at least six months and show cross-reactivity to the Omicron S. However, it remains unknown how the cytotoxicity of cross-reactive CD8+ T cells changes temporally.
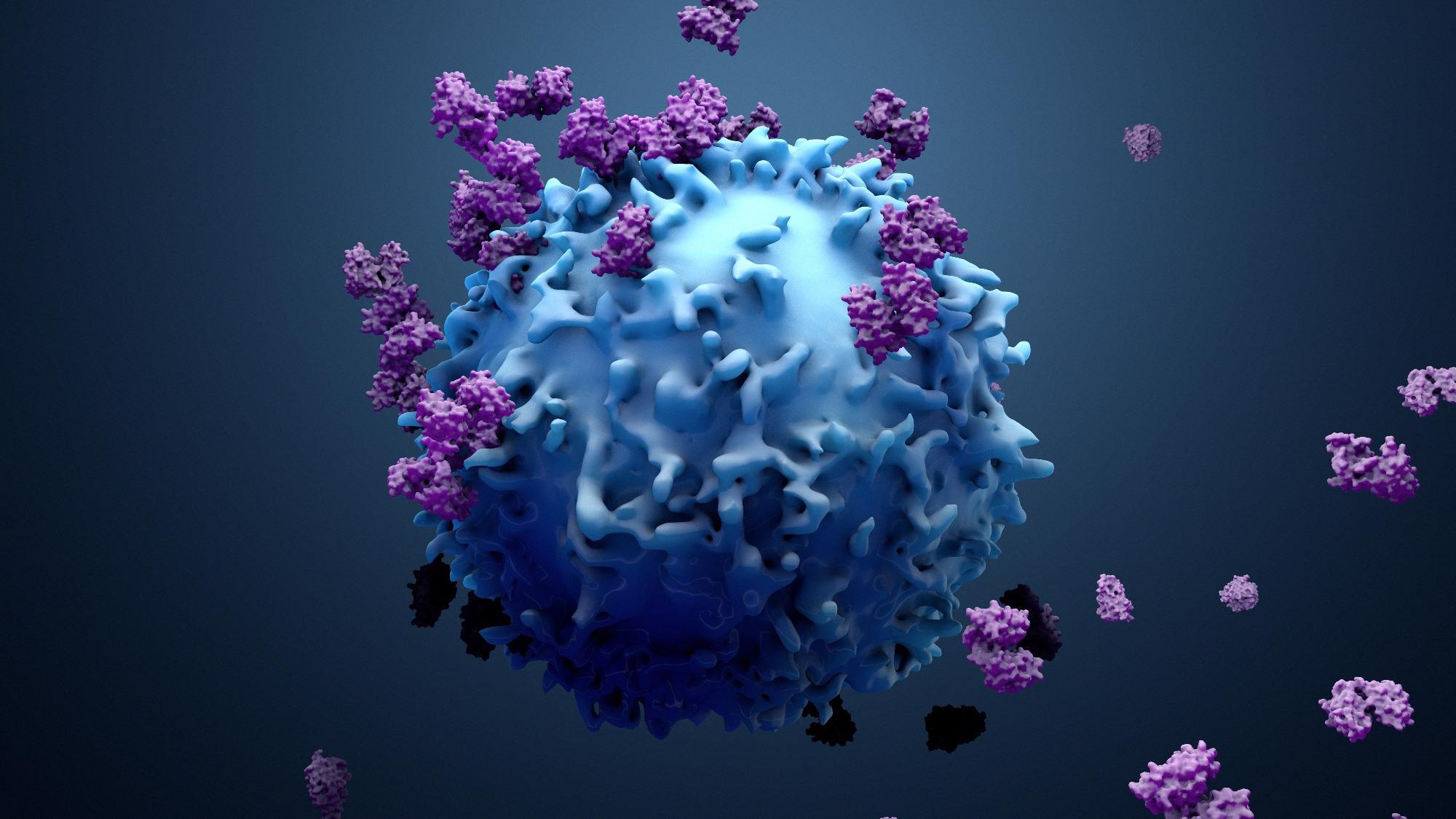 Study: mRNA vaccine induces cytotoxic CD8+ T-cell cross-reactivity against SARS-CoV-2 Omicron variant and regulates COVID-19 severity. Image Credit: Design_Cells/ Shutterstock
Study: mRNA vaccine induces cytotoxic CD8+ T-cell cross-reactivity against SARS-CoV-2 Omicron variant and regulates COVID-19 severity. Image Credit: Design_Cells/ Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
About the study
In the current study, researchers analyzed peripheral blood mononuclear cells (PBMCs) collected from 30 symptomatic COVID-19 patients to identify CD8+ T cell phenotypes that suppressed COVID-19 progression.
First, they examined the cytotoxicity of SARS-CoV-2 S-specific CD8+ T cells in patients with mild disease. Next, they determined whether the BNT162b2 vaccines induced these highly cytotoxic CD8+ T cells.
Flow cytometric (FC) analysis helped the researchers define the total memory-cell population with surface markers such as CD27 and common leukocyte antigen (CD45RO). Likewise, FC showed the antigen-specific-stimulated CD8+ T cell population with CD69 and CD137 markers.
The team also functionally characterized the antigen-specific CD8+ T cells, for which they calculated the cytokine production of CD8+ T cells corresponding to the SARS-CoV-2 S antigen. Finally, they evaluated the cytotoxic activity of SARS-CoV-2 S-specific CD8+ T cells.
The researchers created another study population comprising 21 healthy adults vaccinated with the BNT162b2 vaccine. They collected their samples at three time points: before vaccination, four weeks after the second vaccination, and 12 weeks after the second vaccination.
The team performed an enzyme-linked immunosorbent assay (ELISA) to measure the plasma levels of total immunoglobulin G (IgG)-targeting SARS-CoV-2 S-specific antibodies, in this case, in response to wild-type (WT), Delta, and Omicron S. They used FC analysis to examine CD4+ T cell responses to Delta and Omicron in the BNT162b2-vaccinated healthy donors.
Study findings
SARS-CoV-2 S-specific CD8+ T cells in the acute phase of mild disease simultaneously expressed granzyme A (GZMA), granzyme B (GZMB), and perforin. However, the frequency of these cells diminished three months after the second BNT162b2 vaccination, suggesting that although the mRNA vaccine-induced CD8+ T cells reduced COVID-19 severity, their effect was not long-lasting.
Notably, GZMA and perforin serum levels were higher in SARS-CoV-2-infected patients with mild symptoms than in the healthy individuals and patients with severe COVID-19.
Analyzing the antigen-specific CD8+ T cells via multicolor FC revealed that although cytokine production from these cells in response to antigen stimulation did not vary between mildly and critically ill patients, their expression did. Therefore, profiling the expression of the cytotoxic molecules during SARS-CoV-2 infection could help develop improvised vaccination strategies in the future.
Analyzing CD8+ T cells using a major histocompatibility complex I (MHC-I) multimer showed that the programmed cell death-1 (PD-1)-expressing CD8+ T cells also expressed interferon-gamma (IFN-g). Additionally, these cells expressed activation markers, such as CD38 and human leukocyte antigen – DR isotype (HLA-DR). The authors have emphasized the need for future studies elucidating the association between CD8+ T cell exhaustion and COVID-19 progression.
FC analysis further showed that the frequency of the SARS-CoV-2 S-specific CD8+ T cells was 21% in healthy individuals vaccinated with BNT162b2, suggesting inefficient induction of highly functional cytotoxic CD8+ T cells post-vaccination. The CD8+ T cells subpopulation dipped to 15% three months after the second vaccination. Although they remained reactive to the Delta and Omicron VOCs, their functionality continuously declined.
Conclusions
Taken together, the study findings indicate that although mRNA vaccination induced a subpopulation of CD8+ T cells that might reduce COVID-19 severity, it remains challenging to maintain its effectiveness in the long term.
To increase the effectiveness of future vaccines against existing and emerging SARS-CoV-2 VOCs, the authors recommended incorporating factors that would efficiently induce CD8+ T cells with polyfunctional cytotoxicity that would also persist longer.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Takuto Nogimori, Koichiro Suzuki, Yuji Masuta et al. mRNA vaccine induces cytotoxic CD8+ T-cell cross-reactivity against SARS-CoV-2 Omicron variant and regulates COVID-19 severity. Research Square preprint 2022, DOI: https://doi.org/10.21203/rs.3.rs-1364513/v1, https://www.researchsquare.com/article/rs-1364513/v1
- Peer reviewed and published scientific report.
Nogimori, Takuto, Koichiro Suzuki, Yuji Masuta, Ayaka Washizaki, Mika Yagoto, Mami Ikeda, Yuki Katayama, et al. 2023. “Functional Changes in Cytotoxic CD8+ T-Cell Cross-Reactivity against the SARS-CoV-2 Omicron Variant after MRNA Vaccination.” Frontiers in Immunology 13 (January). https://doi.org/10.3389/fimmu.2022.1081047. https://www.frontiersin.org/articles/10.3389/fimmu.2022.1081047/full.