While the global spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections has slowed, many people suffer long-lasting symptoms, a condition known as post-acute sequelae of COVID 2019 (COVID-19) (PASC), or long COVID. Even though PASC is not widely described, it is most commonly defined as COVID-19 symptoms that continue longer than 30 days.
PASC can manifest as a wide range of symptoms, many exhibiting autonomic characteristics. An autonomic nervous system illness, postural orthostatic tachycardia syndrome (POTS), strongly connected with a prior viral infection, is the most prevalent autonomic diagnosis correlated with PASC. Although autonomic dysfunction is a common consequence of long COVID, the PASC frequency and severity rates remain unclear. Furthermore, while online surveys of PASC patients exist, none have explicitly assessed autonomic symptom load in conjunction with other aspects of the condition.
About the study
The primary purpose of the present study was to determine the incidence and severity of autonomic manifestations in patients with PASC. The authors also evaluated symptom burden in PASC using well-validated questionnaires, which pre-existing comorbidities were linked to a heightened likelihood of autonomic dysfunction, and if the acute COVID-19 severity was correlated with the severity of autonomic dysfunction in this group.
The team performed a global online survey of 2,314 PASC adult patients employing various validated questionnaires, including the composite autonomic symptom score-31 (COMPASS-31), to assess for autonomic dysfunction. Both subjects who tested positive for SARS-CoV-2, i.e., test-confirmed, and those diagnosed with COVID-19 based only on clinical symptoms, i.e., test-unconfirmed, were included in the study. Additional analyses contrasting non-hospitalized and hospitalized individuals were conducted on test-confirmed COVID-19 patients. The researchers examined 53 distinct symptoms over eight different symptom areas to analyze PASC heterogeneity.
Results
The study results demonstrated that there were 87% female participants, higher than earlier studies with 68-75% female patients with PASC. In this adult population research, about 87% of PASC participants were between the ages of 31 and 65, comparable with the age distribution reported in prior studies. The most prevalent symptoms were brain fog, exhaustion, shortness of breath with exercise, headache, palpitations, body pains, tachycardia, and lightheadedness, consistent with previous research that found many of the same symptoms in individuals with PASC.
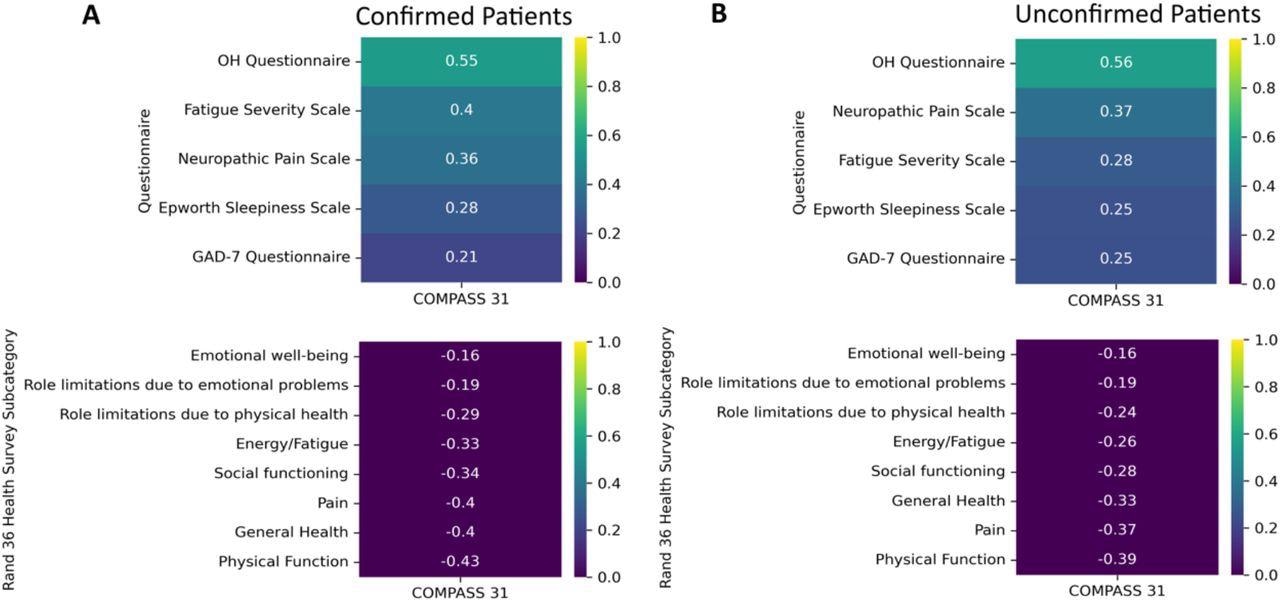
Correlations of the Fatigue Severity Scale, Neuropathic Pain Scale, Epworth Sleepiness Scale, General Anxiety Disorders Assessment, Orthostatic Hypotension Questionnaire and the Rand-36 to total COMPASS-31 scores. * A lower score on the RAND 36-Item Health Survey indicates greater disability.
The test-confirmed SARS-CoV-2 cohort was more probable than the test-unconfirmed group to experience loss of taste and smell. A previous autonomic dysfunction diagnosis was documented in 8.3% of test-unconfirmed COVID-19 patients and 5.1% of test-confirmed patients. POTS was the most often reported autonomic condition, with a prevalence far higher than the expected frequency in the United States (US).
Depression, anxiety, history of vaping or smoking, environmental food or allergies, asthma, hypertension, autoimmune disease history, and obesity were the most often reported pre-existing illnesses in this sample. The frequency of pre-COVID autoimmunity and asthma in the current cohort was far higher than the overall US population, suggesting the potential that these medical disorders might be risk factors for PASC development.
A COMPASS-31 score of above 20 was found in 67% of PASC patients, indicating autonomic dysfunction with moderate to severe. There was no difference in COMPASS-31 scores among test-confirmed non-hospitalized and hospitalized COVID-19 patients. Across all quality-of-life dimensions, both non-hospitalized and hospitalized SARS-CoV-2 patients reported severe functional impairment.
"Our study finds that 67% of individuals with Long COVID are developing dysautonomia. That’s an estimated 38 million Americans with Long COVID dysautonomia, and millions more around the world,” says Lauren Stiles, President of Dysautonomia International and Research Assistant Professor of Neurology at Stony Brook University.
Conclusions
According to the authors, this was the broadest study that used validated autonomic questionnaire scores to show that autonomic dysfunction was frequent in PASC yet available.
In the current sample, the severity of COVID-19 did not link with the degree of autonomic dysfunction, implying that even mild SARS-CoV-2 infections can cause considerable autonomic dysfunction. Furthermore, the autonomic nervous system has a significant role in controlling coagulation pathways and immune function, two factors that seem to engage in long COVID. Hence, the researchers suggest that future research should concentrate on processes of PASC-linked autonomic dysfunction, their correlation to coagulation and immune biomarkers, and potential interventions that can enhance autonomic function.
Overall, the present study findings showed the presence of moderate to severe autonomic dysfunction in all PASC cohorts in this investigation, regardless of hospitalization status, implying that autonomic dysfunction was frequent among the PASC community and not always connected to the severity of acute COVID-19.
"Identifying dysautonomia in Long COVID is important because the autonomic nervous system plays a critical role in regulating immune function, inflammation, coagulation pathways, fatigue, exercise intolerance, cognition, and other factors that appear to play a role in Long COVID. Treatments that improve autonomic nervous system function may offer great benefit in treating the debilitating symptoms of Long COVID," explains Dr. Mitchell Miglis, Associate Professor of Neurology & Neurological Sciences at Stanford University.
"We need the National Institutes of Health to immediately address this crisis and begin funding research aimed at developing effective treatments for Long COVID dysautonomia,” says Jacqueline Rutter, a Dysautonomia International Board Member whose family has been impacted by Long COVID.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Source:
Journal references:
- Preliminary scientific report.
Characterization of Autonomic Symptom Burden in Long COVID: A Global Survey of 2,314 Adults; Nicholas W. Larsen, Lauren E. Stiles, Ruba Shaik, Logan Schneider, Srikanth Muppidi, Cheuk To Tsui, Mitchell G. Miglis, medRxiv preprint 2022, DOI: https://doi.org/10.1101/2022.04.25.22274300, https://www.medrxiv.org/content/10.1101/2022.04.25.22274300v1
- Peer reviewed and published scientific report.
Larsen, Nicholas, et al. "Characterization of Autonomic Symptom Burden in Long COVID: A Global Survey of 2,314 Adults." Frontiers in Neurology, vol. 13, 2022, https://doi.org/10.3389/fneur.2022.1012668, https://www.frontiersin.org/articles/10.3389/fneur.2022.1012668/full