As of May 25, 2022, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus responsible for the coronavirus disease 2019 (COVID-19), has infected more than 526 million people and caused over 6.28 million deaths worldwide.
Scientific and clinical evidence has shown the presence of potential post-acute and long-term effects of SARS-CoV-2 infection in multiple organ systems. Previous research has primarily focused on small samples of patients or specific populations.

Study: Understanding Post-Acute Sequelae of SARS-CoV-2 Infection through Data-Driven Analysis with the Longitudinal Electronic Health Records: Findings from the RECOVER Initiative. Image Credit: sasirin pamai / Shutterstock.com

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
A new study available on the medRxiv* preprint server characterizes post-acute sequelae of SARS-CoV-2 infection (PASC) using data from two large national patient-centered clinical research networks (PCORnet), which include 11 million patients in New York City (NYC) and 16.8 million patients in Florida.
Drawbacks of existing studies
Recently, many retrospective cohort analyses have described PASC using real-world patient data; however, there are two key limitations of these existing studies.
First, the disease etiology and pathophysiology of PASC are complicated, thereby implying that a conventional hypothesis-driven study design may result in biased findings. Further, these studies have typically been conducted on small sample sizes or specific patient populations, which raises questions about the generalizability of these results.
About the study
The current study overcomes the aforementioned challenges by developing a high-throughput causal inference pipeline to identify potential PASC symptoms. This study is part of the United States National Institutes of Health (NIH) Researching COVID to Enhance Recovery (RECOVER) Initiative.
Herein, researchers used electronic health records (EHR) from two large national PCORnets: INSIGHT and OneFlorida+. Whereas INSIGHT covers patients in the New York City (NYC) metropolitan area, OneFlorida+ covers patients from Florida, Georgia, and Alabama. A total of 137 potential PASC diagnoses and 459 potential PASC medications were considered.
The researchers built an outcome-specific cohort with patients who were free of diagnoses or medications at baseline for each diagnosis and medication. Next, an inverse propensity treatment re-weighting (IPTW) was applied to adjust for confounders and an adjusted hazard ratio and excess burden in the post-acute phase of infection were calculated. Only new incidences in the post-acute period were considered, as this provided the most efficient way to define PASC phenotypes.
Study findings
A range of diagnoses and medications were found to be consistent with higher adjusted hazard ratios and excess burdens in SARS-CoV-2 infected patients with respect to non-infected individuals. PASC was observed to be a multi-organ disease, as the diagnoses and medications spanned a wide range of organ systems.
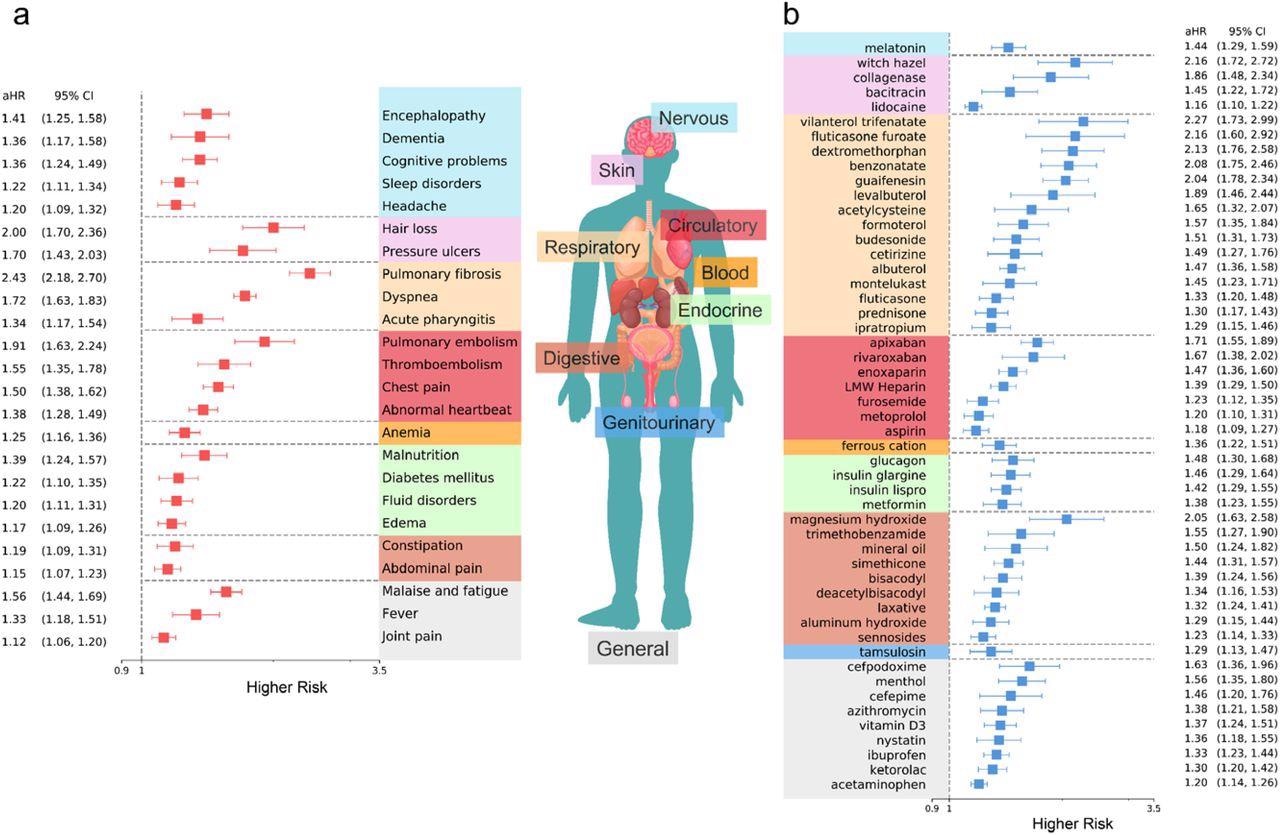
Identified potential incident PASC conditions from the INSIGHT cohort, March 2020 to November 2021. a. The adjusted hazard ratios of incident diagnoses. b. The adjusted hazard ratios of incident use of medications. The sequelae outcomes were ascertained from day 30 after the SARS-CoV-2 infection and the adjusted hazard ratio was computed at 180 days after the SARS-CoV-2 infection. The colors represent different organ systems.
Diagnoses included respiratory, dermatologic, cardiovascular, nervous, and other problems. Additionally, an increased incident prescription risk in a diverse set of medications was observed by scientists, some of which included drugs for asthma, cough, anticoagulants, and constipation.
The adjusted excess burden of different potential PASC diagnoses was analyzed across a diverse set of groups. To this end, hospitalized patients reported more excess cases of potential PASC diagnoses and medications in both the INSIGHT and OneFlorida+ cohorts.
Female, older, and non-white patients had higher excess cases of PASC conditions. Comorbidity status also played an important role, although dyspnea consistently showed the highest excess burden. A greater number of potential PASC conditions were identified in patients with cardiac problems, type II diabetes, and chronic kidney disease (CKD).
Overall, adjusted hazard ratios (aHRs) identified from the INSIGHT cohort were higher than in the OneFlorida+ cohort. Specifically, the rates of thromboembolism and pulmonary fibrosis were 50% greater in the INSIGHT cohort.
Nine diagnoses and nine medications were identified in the OneFlorida+ cohort as compared to 25 diagnoses and 51 medications in the INSIGHT cohort. The heterogeneity in the results could be caused by different infection periods and patient characteristics.
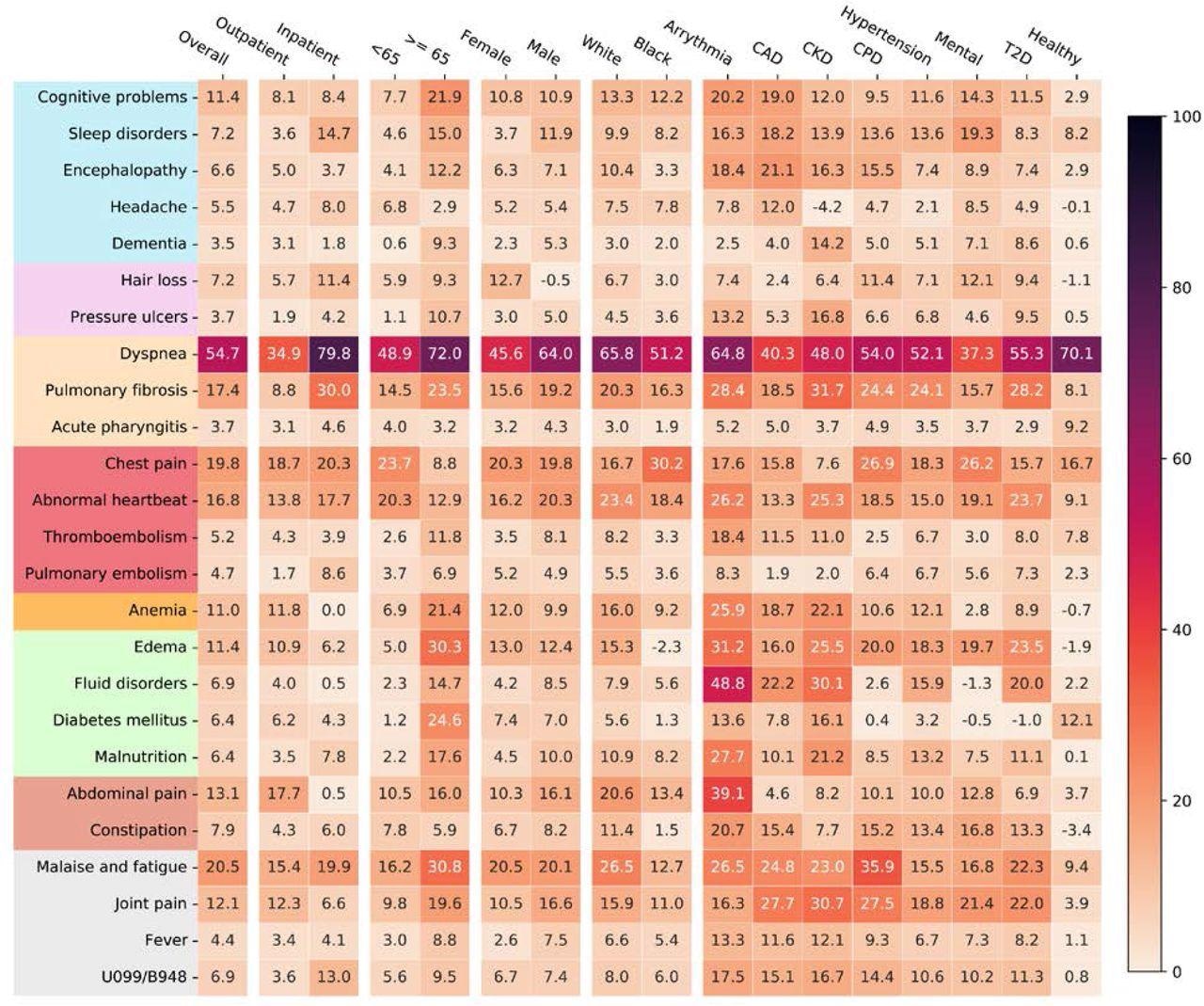
Adjusted excess cumulative incidence of post-acute sequelae of SARS-CoV-2 infection (PASC) in the INSIGHT cohort, from March 2020 to November 2021, stratified by the acute severity status, age groups, gender, race groups, and baseline pre-existing conditions. P-value < 3.6 × 10−4were used for selecting significant diagnoses. Different color panels represent different organ system, including (from top to bottom): nervous system, skin, respiratory system, circulatory system, blood forming organs, endocrine and metabolic, digestive system, genitourinary system, and general signs. CAD, coronary artery disease; CKD, chronic kidney disease; CPD, chronic pulmonary disease; T2D, diabetes type 2; Healthy: no documented pre-existing conditions and no PASC-like symptoms at baseline. Two ICD-10 diagnosis codes B948 (sequelae of other specified infectious and parasitic diseases) and U099 (post COVID-19 condition, unspecified) were also used to compare general post-acute sequelae of SARS-CoV-2 infection in different groups.
Strengths and limitations
Key strengths of this study include the data-driven approach and the large population of general adult patients. Further, the researchers utilized data from two large-scale clinical research networks covering diverse sets of patients, which revealed the heterogeneity of PASC manifestations, thus improving generalizability. Furthermore, since the United States experienced multiple COVID-19 waves during the enrollment period, the results highlight the different epidemiological and clinical characteristics.
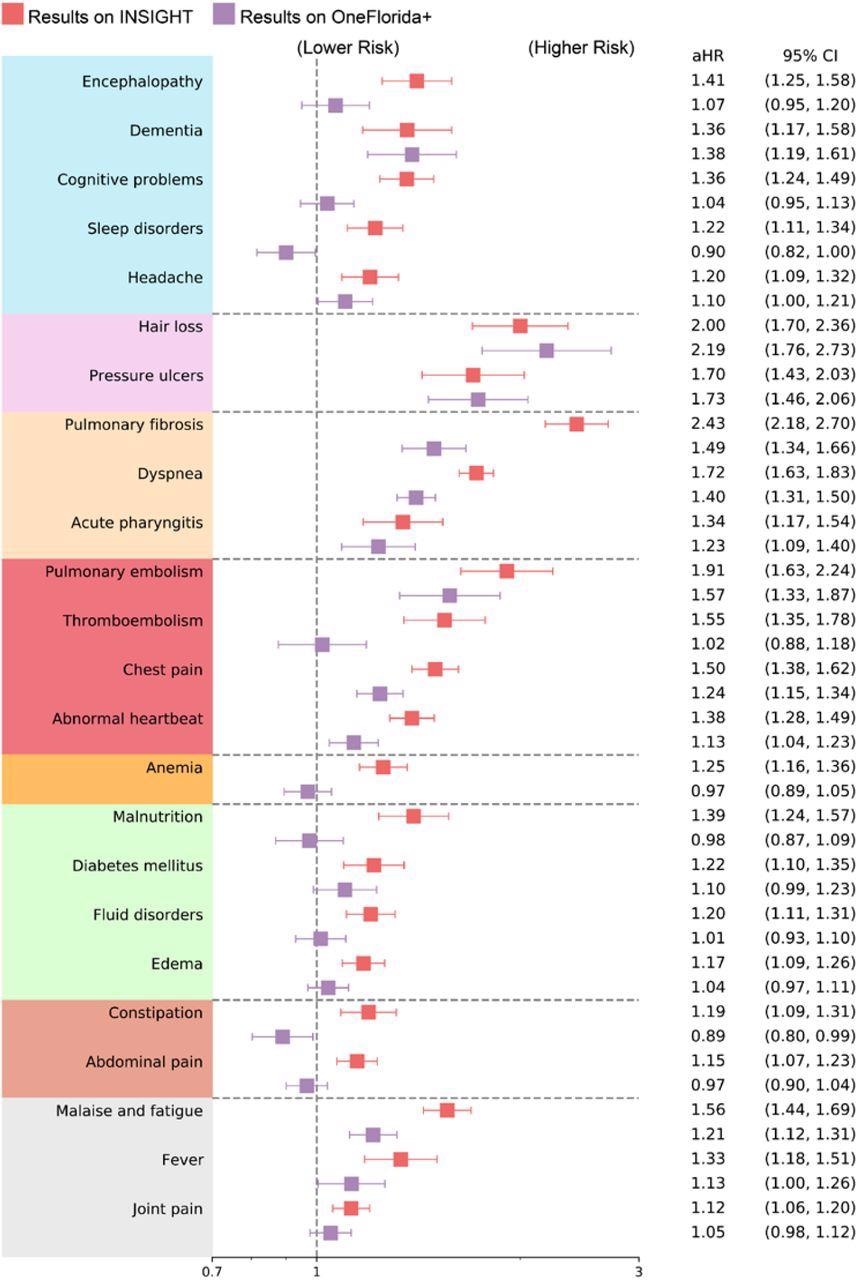
Comparison of the post-acute sequelae of SARS-CoV-2 risks in the INSIGHT cohort versus in the OneFlorida+ cohort, from March 2020 to November 2021. Adjusted hazard ratios were reported. The color panels represent different organ system, including (from top to bottom): nervous system, skin, respiratory system, circulatory system, blood-forming organs, endocrine and metabolic, digestive system, and other general signs.
The current study also has a few limitations. Firstly, the exposure group was not randomized, although the researchers balanced hypothetical confounders and obtained consistent results.
An additional limitation was that the participants resided in NYC and Florida, which might not be representative of other populations. Third, the study only considered incident events, while leaving the worsening and relapsing conditions for future research.
A final limitation was that the study period did not allow for the inclusion of patients infected during the phase dominated by the Omicron variant and did not include information on vaccination status.
Conclusions
The researchers observed that adults surviving beyond 30 days of their COVID-19 diagnosis showed high incident risks and burdens. Furthermore, PASC was found to be a complex condition that involves multiple organ systems. Significant heterogeneity was observed across geographical regions and patient sub-groups.
Taken together, the study findings further our understanding of PASC and highlight the need for more research to inform the diagnosis and prevention of PASC.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Zang, C., Zhang, Y., Xu, J., et al. (2022) Understanding Post-Acute Sequelae of SARS-CoV-2 Infection through Data-Driven Analysis with the Longitudinal Electronic Health Records: Findings from the RECOVER Initiative. medRxiv. doi:10.1101/2022.05.21.22275420. https://www.medrxiv.org/content/10.1101/2022.05.21.22275420v2
- Peer reviewed and published scientific report.
Zhang, Hao, Chengxi Zang, Zhenxing Xu, Yongkang Zhang, Jie Xu, Jiang Bian, Dmitry Morozyuk, et al. 2022. “Data-Driven Identification of Post-Acute SARS-CoV-2 Infection Subphenotypes.” Nature Medicine, December, 1–10. https://doi.org/10.1038/s41591-022-02116-3. https://www.nature.com/articles/s41591-022-02116-3.