The coronavirus disease (COVID-19) pandemic has imposed operational burdens on infectious disease epidemiology, thus preventing their routine monitoring. Despite these challenges, continuous surveillance of the influenza virus is required for the production of new vaccines each year.
The symptoms of both COVID-19 and influenza are quite similar, as both the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the influenza virus target the respiratory system. A notable difference between these two viruses is that SARS-CoV-2 uses the angiotensin-converting enzyme 2 (ACE2) receptor on epithelial and endothelial cells to gain entry, while the influenza virus uses sialic acid groups on surface glycoproteins of epithelial cells.
Study: Epidemiological Interactions of Influenza and SARS-CoV-2 within a University Population During Omicron B.1.1.529 Outbreak. Image Credit: Adao / Shutterstock.com

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
A new study published on the preprint server medRxiv* identifies the potential correlations that exist between SARS-CoV-2 and influenza infections.
About the study
The current study involved the collection of anterior nasal swabs from both symptomatic and non-symptomatic individuals at separate facilities. Individuals who were experiencing COVID-19 symptoms, as well as those who came in close contact with an individual who was positive for COVID-19, were required to submit their samples at the symptomatic site.
A multiplex reverse transcription-quantitative polymerase chain reaction (RT-qPCR) assay was carried out to monitor the incidence of COVID-19, Influenza A, and Influenza B among symptomatic individuals.
Study findings
A total of 3,065 individuals were tested between November 1, 2021, and February 28, 2022. The first Influenza A case was detected on November 4, 2021, during which the average weekly prevalence rate was 13.62%.
Between December 27, 2021, and January 7, 2022, a sharp decrease in Influenza A cases at a rate of 12.5% was observed, while SARS-CoV-2 cases increased at a rate of 3.75%. Notably, the rapid spread of the SARS-CoV-2 Omicron B.1.1.529 variant was associated with the reduced incidence of influenza cases.
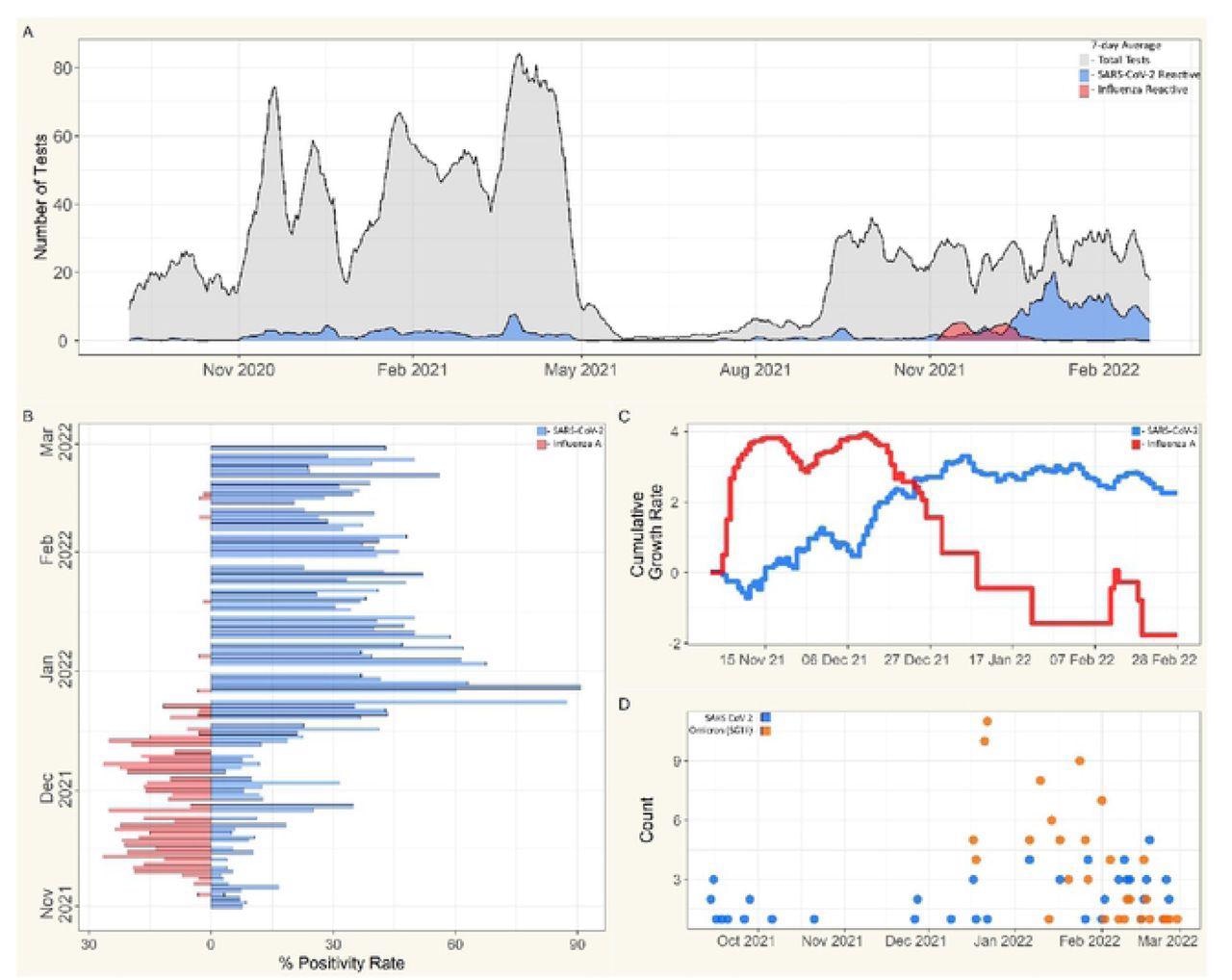 A) Seven-day averages for RT-qPCR testing collected from symptomatic individuals; tests collected, grey, reactive for SARS-CoV-2, blue, reactive for Flu A, red. B) Positivity rate for symptomatic cohort from November 1st, 2021,. to February 28th, 2022; SARS-CoV-2, blue; Flu A. red. C) Cumulative growth rates for seven-day averages of SARS-CoV-2 and influenza incidence in symptomatic cohort from November 1st. 2021. to February 28th, 2022; SARS-CoV-2. blue; Flu A. red. D) Totals of SARS-CoV-2 Omicron (B.1.1.529) variant determination via S-gcnc target failure (SGTF) for symptomatic population from September 14th, 2021, to February 28th 2022; SARS-CoV-2, blue; SGTF, orange, n=172.
A) Seven-day averages for RT-qPCR testing collected from symptomatic individuals; tests collected, grey, reactive for SARS-CoV-2, blue, reactive for Flu A, red. B) Positivity rate for symptomatic cohort from November 1st, 2021,. to February 28th, 2022; SARS-CoV-2, blue; Flu A. red. C) Cumulative growth rates for seven-day averages of SARS-CoV-2 and influenza incidence in symptomatic cohort from November 1st. 2021. to February 28th, 2022; SARS-CoV-2. blue; Flu A. red. D) Totals of SARS-CoV-2 Omicron (B.1.1.529) variant determination via S-gcnc target failure (SGTF) for symptomatic population from September 14th, 2021, to February 28th 2022; SARS-CoV-2, blue; SGTF, orange, n=172.
The current study indicated an inverse relationship between SARS-CoV-2 and influenza infection cases. Thus, healthcare providers must employ more complete respiratory panels to monitor strain dominance and the prevalence of coinfections with both viruses.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.