In a recent study posted to the bioRxiv* pre-print server, researchers analyzed two genomic sequences of the Monkeypox virus from Belgium and Portugal termed ITM001 and PT0001, respectively, to show that the May 2022 Monkeypox outbreak most likely originated from the West African clade of the virus. Moreover, these sequences were ~99% identical to Monkeypox sequences derived from the cases between 1971 and 2017.
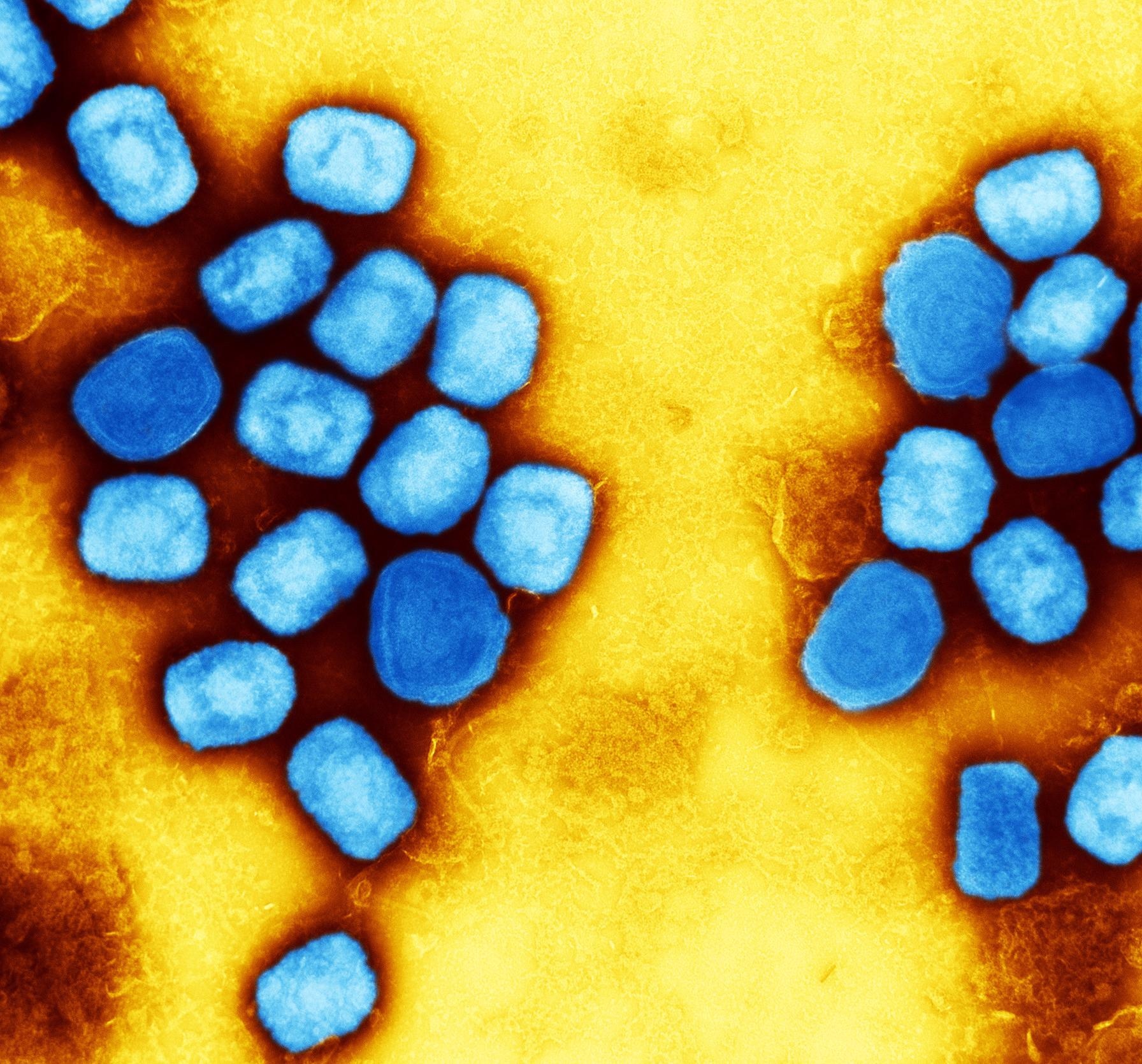 Study: Genomic characterization of the recent monkeypox outbreak. Image Credit: NIAID
Study: Genomic characterization of the recent monkeypox outbreak. Image Credit: NIAID

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Background
In May 2022, there were around 100 cases of Monkeypox-caused infections in 12 countries, including Australia, France, Germany, Belgium, Canada, Italy, Sweden, Netherlands, United Kingdom, United States, Portugal, and Spain. In addition, the world is facing a pandemic due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Although the Monkeypox cases did not claim lives or surge to high numbers as SARS-CoV-2; yet, it is crucial to strictly monitor the genomic features and etiology of the Monkeypox virus to evade any imminent potential threat.
About the study
In the present study, researchers queried for the PT0001 Monkeypox genome sequence in the basic local alignment search tool (BLAST) and retrieved 100 sequences most similar to genomic sequences from Monkeypox virus cases that occurred in May 2022 in Portugal and Belgium.
The BLAST-retrieved sequences belonged to 28 Cowpox and 72 Monkeypox sequences, dating back to 1971. The researchers added genome sequences of the Central African Monkeypox virus and the Indian-origin Variola virus as the two reference sequences to this selection.
They also analyzed specific genomic sequences of Monkeypox and related viruses for proteins of relevance using the Protein Data Bank, a storehouse of viral protein structures. First, the team analyzed the A42R protein, a 130 amino acid (AA) long protein involved in cytoskeletal structure and function, from the Central African Monkeypox strain Zaire-96-I-16. Likewise, they extracted H3L proteins from PT0001 and ITM001 and compared them with representative database sequences for West African Monkeypox, Central African Monkeypox, Cowpox, and Variola viruses.
Study findings
Phylogenetic analysis showed that the PT0001 and ITM001 sequences from Portugal and Belgium resembled the West African clade of the Monkeypox virus. While Cowpox genomes constituted a different genetic group, the Variola virus genome was highly similar to the Monkeypox virus. It possessed over 95% DNA identity with both Monkeypox clades and the analyzed Cowpox and Variola virus genome sequences.
Furthermore, the authors noted a 100% similarity between PT0001 and ITM001 Monkeypox sequences and the other Monkeypox A42R proteins. The authors observed variations in only four AAs between Monkeypox A42R sequences and related Orthopoxviruses, viz., Lysine 16, Valine 48, Phenylalanine 66, and Histidine 55. These four AAs are located outside or on the alpha-helices and beta-sheets border, hence could not cause a major structural rearrangement of the A42R protein. While multiple sequence alignment showed a high similarity between H3L sequences of all the viruses; however, 21 AAs differed between the Monkeypox and the Variola virus in H3L, suggesting a higher variance for this protein compared to A42R.
H3L is a 324 AA long glycosyltransferase located on the viral envelope and plays a key role in the attachment to a host cell and subsequent poxvirus entry. Studies have shown that antibodies induced by a smallpox vaccine bind H3 proteins, and the cluster of differentiation (CD8)+ T cells recognize H3L as an antigen, indicating its immunological significance.
Therefore, the Monkeypox H3, similar to SARS-CoV-2 spike (S) protein, is an ideal vaccine target. The anti-S messenger ribonucleic acid (mRNA)-based SARS-CoV-2 vaccines have proved most successful in combating coronavirus disease 2019 (COVID-19). Likewise, the similarity of H3 in the Variola and Monkeypox viruses is most likely responsible for the efficacy of smallpox vaccines in protecting against Monkeypox. It is noteworthy that Monkeypox affects humans just as smallpox and both these viruses are members of the Orthopoxvirus family. While the Variola virus has been eradicated worldwide, unfortunately, the Monkeypox virus is still endemic in Africa.
Conclusions
Thankfully, the recent Monkeypox outbreak did not result in any casualties. Moreover, the authors did not find any genetic divergence in the recently identified and historic Monkeypox virus strains, pointing out that this disease is unlikely to attain pandemic status. Nevertheless, continuous and careful surveillance of the evolution of Monkeypox H3 proteins is of paramount importance to monitor the Monkeypox virus evolution during this outbreak and in the future and to develop effective vaccines against this disease.

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.