In a recent study posted to the medRxiv* pre-print server, researchers investigated coronavirus disease 2019 (COVID-19) incidence and severity among systemic autoimmune rheumatic diseases (SARDs) patients in Massachusetts, United States (US), between March 1, 2020, and January 31, 2022.
 Study: Temporal trends in COVID-19 outcomes among patients with systemic autoimmune rheumatic diseases: From the first wave to Omicron. Image Credit: Adao / Shutterstock
Study: Temporal trends in COVID-19 outcomes among patients with systemic autoimmune rheumatic diseases: From the first wave to Omicron. Image Credit: Adao / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Background
Some people with SARDs are at high risk of progressing to severe COVID-19, resulting in subsequent hospitalization and death. SARD patients suffer from underlying medical conditions, including suppressed immunity and end-organ damage contributing to poor immune responses to natural severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and vaccination.
Previous studies investigated temporal trends in COVID-19 outcomes among SARD patients before the Omicron wave. For instance, a Swedish study showed patients with inflammatory joint diseases had worse COVID-19 clinical outcomes than the general population early in the pandemic.
However, the authors hypothesized that COVID-19 vaccination, testing, and treatments may have contributed to improved temporal COVID-19 outcomes among people with SARDs during the most recent Omicron wave in the US. So they investigated whether clinical COVID-19 outcomes have improved in recent periods for patients with SARDs.
About the study
In the present study, researchers computed weekly counts of total COVID-19 cases, including severe cases, to compare them by calendar period and vaccination status across five-time frames spanning from the first infection wave through the Omicron wave. They used logistic regression to estimate the odds ratio (ORs) for severe COVID-19 for each period compared to the earlier reference period.
The researchers also explored other notable trends among patients with SARDs during the ongoing pandemic. But, more importantly, they assessed whether each case of death among SARD patients was due to underlying immunosuppression or other comorbidities.
Study findings
The authors identified 1449 SARD patients who suffered from COVID-19, of which 399 cases were severe. The mean age of the patients was 58.4 years, 75.2% were female, and 33.9% also suffered from rheumatoid arthritis. Over time, the proportion of severe COVID-19 outcomes declined. The adjusted ORs of severe COVID-19 in the Omicron wave was 0.29; however, the absolute number of severe COVID-19 cases during the peak of the Omicron variant wave was similar to the peaks of other waves.
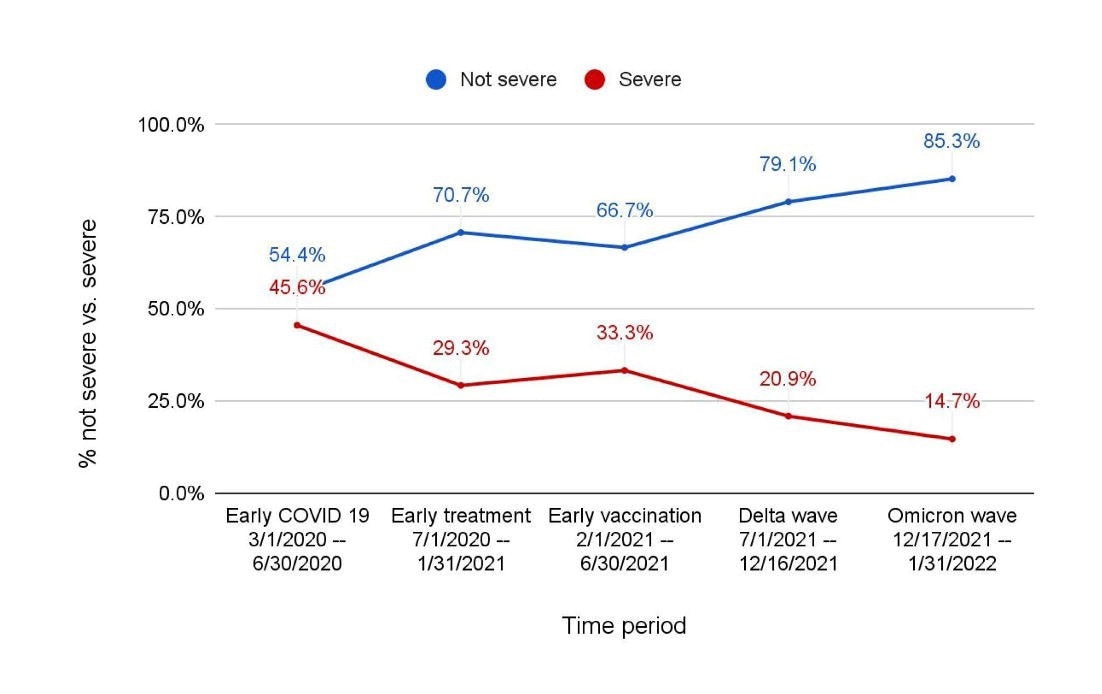
Accordingly, 45.6% of cases displayed severity between March 1 and June 30, 2020, but only 14.7% were severe between December 17, 2021, and January 31, 2022. The case severity was higher among unvaccinated SARDs patients compared to unvaccinated patients (78.4% vs. 59.5%). Notably, some patients with SARDs were hospitalized or died during the Omicron wave. These patients tended to have other comorbidities (e.g., interstitial lung disease, malignant tumors). These findings highlight the need for ongoing risk mitigating strategies for many SARDs patients that may be related to SARD or its treatment.
Regarding other than temporal trends, the authors noted a decrease in the proportion of SARDs patients with COVID-19 who identified themselves as Black or Hispanic. The patient's age also decreased during the study period. Several factors, including changes in access to diagnostics and treatments, and vaccination, could have contributed to these trends. The shift in diagnostics, e.g., diagnosing infections using rapid antigen tests at home, will make it increasingly tedious to capture mild SARS-CoV-2 infections for epidemiologic studies in SARD patients. More importantly, leveraging electronic health record data will remain important in capturing such trends among these patients in future studies.
Conclusions
The study demonstrated a steep decline in severe COVID-19 cases among SARD patients from early in the pandemic to recent periods, including the Omicron wave. These temporal improvements in adverse COVID-19 clinical outcomes were likely multifactorial. Advances in COVID-19 testing, prevention and treatment strategies likely improved adverse clinical outcomes among SARD patients. Additionally, improved hospital capacity, a decrease in the number of vulnerable individuals, and decreased virulence of SARS-CoV-2 variants further improved temporal outcomes in SARD patients.
Interestingly, although vaccination benefitted many SARD patients with immunosuppressants, it is likely that they may still be vulnerable to severe COVID-19. Future studies should expand the observations of the present study to future SARS-CoV-2 variants and consider waning immunity among SARD patients following vaccination or natural infection. Pre-exposure prophylaxis with tixagevimab/cilgavimab, a monoclonal antibody against SARS-CoV-2, represents an important strategy for protecting high-risk patients. Therefore, future studies should also evaluate the real-world effectiveness of tixagevimab/cilgavimab in patients with SARD.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Temporal trends in COVID-19 outcomes among patients with systemic autoimmune rheumatic diseases: From the first wave to Omicron, Yumeko Kawano, Naomi J. Patel, Xiaosong Wang, Claire E. Cook, Kathleen M.M. Vanni, Emily N. Kowalski, Emily P. Banasiak, Grace Qian, Michael DiIorio, Tiffany Y.-T. Hsu, Michael E. Weinblatt, Derrick J. Todd, Zachary S. Wallace, Jeffrey A. Sparks, medRxiv pre-print 2022, DOI: https://doi.org/10.1101/2022.06.19.22276599, https://www.medrxiv.org/content/10.1101/2022.06.19.22276599v1
- Peer reviewed and published scientific report.
Kawano, Yumeko, Naomi J. Patel, Xiaosong Wang, Claire E. Cook, Kathleen MM Vanni, Emily N. Kowalski, Emily P. Banasiak, et al. 2022. “Temporal Trends in COVID-19 Outcomes among Patients with Systemic Autoimmune Rheumatic Diseases: From the First Wave through the Initial Omicron Wave.” Annals of the Rheumatic Diseases 81 (12): 1742–49. https://doi.org/10.1136/ard-2022-222954. https://ard.bmj.com/content/81/12/1742.