Immune correlates may have a role in protective immunity mechanistically. Yet, they can also indicate substitutes for other immunological systems vital for anti-pathogen control. Immune correlates towards SARS-CoV-2 are commonly determined at maximal immunogenicity after vaccination. Nonetheless, immune responses that elevate specifically during the anamnestic response after infection can offer comprehensive and mechanistic details regarding the immune pathways of protection. Furthermore, it is unknown if anamnestic correlates are shared by the SARS-CoV-2 VOCs, such as the Delta and more remote Omicron VOCs.
About the study
In the present study, the investigators thoroughly evaluated the humoral immune reaction in COVID-19 vaccinated people who had recently contracted either the Omicron or Delta VOC infections to characterize the anamnestic markers of immunity among SARS-CoV-2 VOCs.
A significant association exists between non-neutralizing antibody effector patterns and the natural resolution of severe COVID-19. In light of this connection, the team conducted systems serology on the sera of 37 and 23 subjects who had completed their SARS-CoV-2 vaccination series and had a recorded breakthrough infection of the Delta or Omicron VOCs, respectively, one week and two to three weeks after infection. They sought to identify the particular humoral traits connected to the resolution of infection.
Further, the authors assessed the fold rise in immunoglobulin G1 (IgG1) concentrations throughout subdomains of the SARS-CoV-2 spike (S) protein, VOCs, and common human CoVs (HCoVs). This was to compare the degree of the anamnestic expansion among S domains throughout the breakthrough instances. They used partial least squares discriminant analysis (PLS-DA) on antibody reactions obtained in breakthrough cases two to three weeks after infection to determine a minimal multivariate fingerprint of Omicron or Delta breakthrough infections across vaccinated persons.
Breakthrough cases were divided among people who got either of the two COVID-19 messenger ribonucleic acid (mRNA) vaccinations (mRNA-1273 (Moderna) or BNT162b2 (Pfizer)). This was to see if they produced an identical anamnestic reaction. Additionally, the team mapped the broadening breakthrough infection response among peptides covering the S antigen's S2 domain to determine whether S2-specific reactions targeted distinct areas of S2.
Results
The study results indicated that after the Omicron and Delta breakthrough infections, a limited transient SARS-CoV-2 N-terminal domain (NTD) and receptor-binding domain (RBD)-specific immune enhancement was seen. On the contrary, one week following the breakthrough infection, opsonophagocytic S-specific antibody reactions exhibited a remarkable immunodominant expansion, focusing primarily on the conserved SARS-CoV-2 S2-domain.
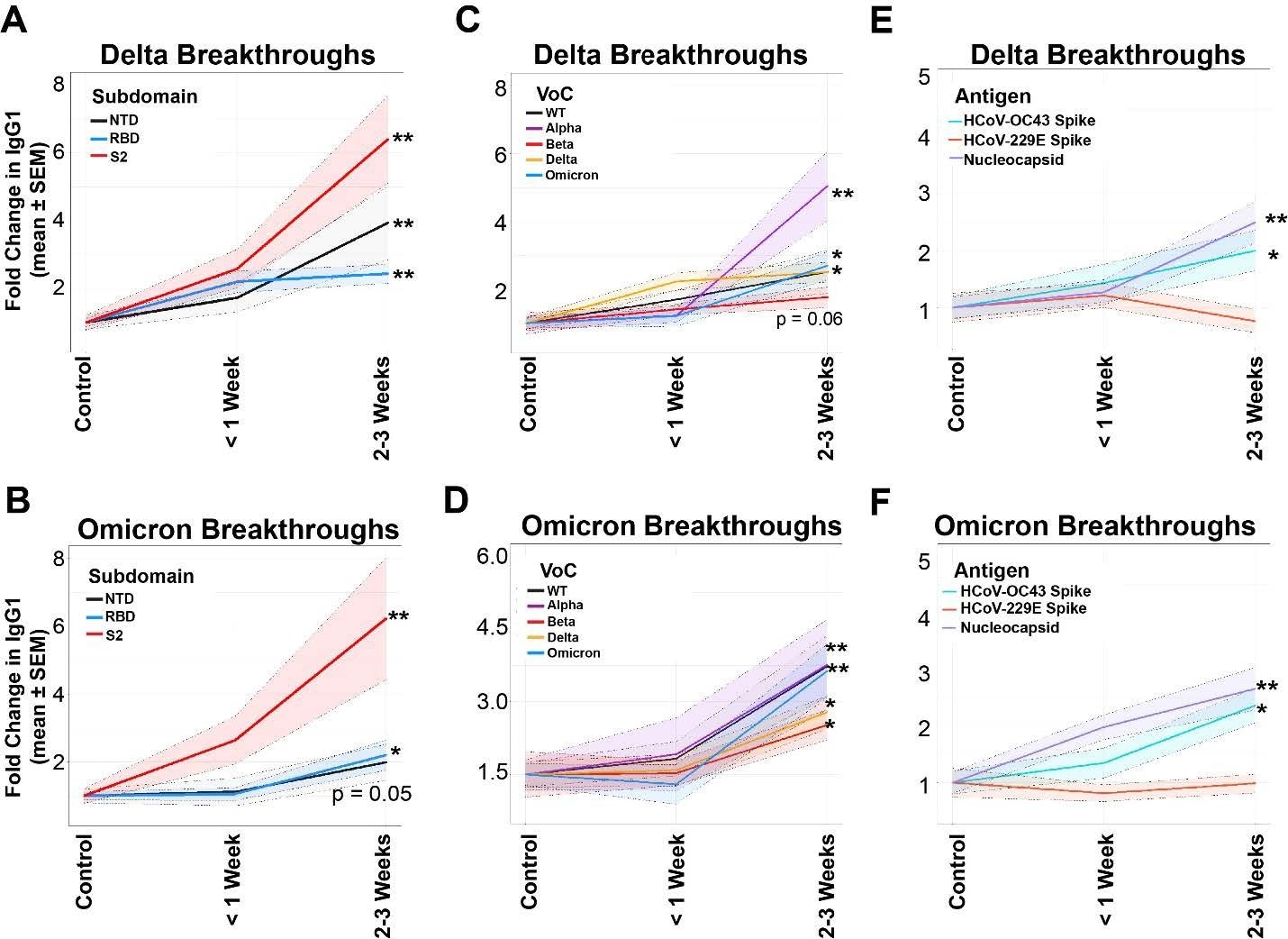 Conserved regions of Spike are selectively expanded in breakthrough cases. (A) Fold changes in IgG1 binding of the subdomains of Spike (NTD in black, RBD in blue, and S2 in red) for vaccinated, Delta breakthrough cases at <1 week or 2-3 Weeks post-breakthrough. (B) Same as A, but for vaccinated Omicron breakthrough cases. (C) Fold changes in IgG1 binding of the full-length Spikes from VoC in Delta breakthrough cases. (D) Same as C, but for Omicron breakthrough cases. (E) Fold changes in IgG1 binding of the Spike of common CoV Spikes in Delta breakthrough infections at < 1 Week or 2-3 Weeks post-breakthrough. SARS-CoV-2 nucleocapsid (N) is used as a control for infection. (F) Same as C, but for Omicron breakthroughs. * = p < 0.05, and ** = p < 0.01 for all panels.
Conserved regions of Spike are selectively expanded in breakthrough cases. (A) Fold changes in IgG1 binding of the subdomains of Spike (NTD in black, RBD in blue, and S2 in red) for vaccinated, Delta breakthrough cases at <1 week or 2-3 Weeks post-breakthrough. (B) Same as A, but for vaccinated Omicron breakthrough cases. (C) Fold changes in IgG1 binding of the full-length Spikes from VoC in Delta breakthrough cases. (D) Same as C, but for Omicron breakthrough cases. (E) Fold changes in IgG1 binding of the Spike of common CoV Spikes in Delta breakthrough infections at < 1 Week or 2-3 Weeks post-breakthrough. SARS-CoV-2 nucleocapsid (N) is used as a control for infection. (F) Same as C, but for Omicron breakthroughs. * = p < 0.05, and ** = p < 0.01 for all panels.
This S2-specific functional humoral reaction, which primarily targets common CoVs and numerous SARS-CoV-2 VOCs, continued to develop over two to three weeks after both Omicron and Delta breakthrough infections. These reactions were focused drastically on the fusion peptide 2 (FP2) and heptad repeat 1 (HR1), and both FP2 and HR1 were linked to faster viral clearance rates.
A distinctive anamnestic rise of early S2 FP2- and HR1-specific IgM antibodies leveraging monocyte phagocytosis was responsible for most S-specific expansion. Further, in both Omicron and Delta breakthrough infections, a more mature S2 HR1- and FP2-specific IgG fraction crystallizable receptor (FcR) attaching neutrophil recruiting response was observed. These data suggested an unexpected and crucial role for S2-specific functional humoral immunity as important anamnestic markers of immunity throughout SARS-CoV-2 VOCs. This inference was contrary to the immunodominant vaccine-triggered reaction to the RBD.
The authors noted discrepancies in the anamnestic reflex post-Pfizer and Moderna vaccination. They found an elevated magnitude advancement of anamnestic immunity in Pfizer vaccinees and a functional augmentation in Moderna vaccinees. Nevertheless, both breakthrough characteristics led to an expansion of immunity specific to the S2 domain.
The variations in vaccination data might be associated with the differences in real-world efficacy among the vaccine platforms. Indeed, the Moderna vaccinees demonstrated decreased breakthrough infections, possibly linked with the elevated functional humoral immunity and IgA concentrations, likely imparting a notably robust defense against SARS-CoV-2 infection at the mucosal barrier. Yet, the increase of S2-specific immunity after both vaccinations targeting HR1 and FP2 might be connected to their accessible sites on the S protein.
Conclusions
The current research evaluated the post-COVID-19 immunological patterns that emerged in breakthrough infections with a specific focus on determining if the kinetics of breakthrough markers of immunity were constant among the SARS-CoV-2 VOCs. The study findings showed a quick expansion of FcR attaching and opsonophagocytic humoral immune reactions across the Omicron and Delta VOC breakthrough cases, with a coherent priority for the expansion of the S protein S2 subdomain centered on the FP2 and HR1, which tracked with augmented SARS-coV-2 clearance.
Taken together, the present study indicates that the control of SARS-CoV-2 infection among VOCs was critically dependent on highly conserved, effective S2-specific reactions. The current work implies that humoral response connected to viral attenuation could direct next-generation COVID-19 vaccine boosting techniques to provide extensive protection against future SARS-CoV-2 VOCs.

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Journal reference:
- Preliminary scientific report.
Anamnestic Humoral Correlates of Immunity Across SARS-CoV-2 Variants of Concern; Ryan McNamara, Jenny S Maron, Harry L Bertera, Julie Boucau, Vicky Roy, Amy K. Barczak, The Positives Study Staff, Nicholas Franko, Jonathan Z Li, Jason S McLellan, Mark Siedner, Jacob E Lemieux, Helen Chu, Galit Alter, bioRxiv preprint 2022, DOI: https://doi.org/10.1101/2022.06.19.496718, https://www.biorxiv.org/content/10.1101/2022.06.19.496718v1