Currently, there is a lack of understanding of the factors that drive the neuropsychiatric symptoms present during acute and long-term COVID-19. Studies have shown a correlation between the kynurenine pathway metabolites, such as quinolinic acid (QUIN) and 3-hydroxykynurenine (3-HK), and COVID-19 severity. Therefore, they could potentially serve as biomarkers of neuropsychiatric long COVID symptoms.
Some pathogenic infections, including COVID-19 and subsequent inflammatory conditions, can alter the activity of the enzymes of the kynurenine pathway. QUIN is glutamatergic N-methyl-D78 aspartate (NMDA) receptor antagonist, and its high concentrations induce excitotoxic neuronal death. Conversely, kynurenic acid (KYNA), an antagonist of NMDA-receptor, prevents excessive calcium influx in a cell. On the other hand, 3-HK is neurotoxic and pro-inflammatory, promotes the generation of reactive oxygen species (ROS), and accelerates endothelial cell apoptosis.
While a blood-brain barrier (BBB) partially prohibits the entry of QUIN and KYNA into the central nervous system (CNS), 3-HK and KYN, a metabolite produced from kynurenine pathway-mediated tryptophan (TRP) metabolism, can freely pass the BBB. The SARS-CoV-2 infection affects the KYN levels by inducing the production of the pro-inflammatory cytokine, interferon-gamma (IFN-ɣ) that stimulates the kynurenine pathway enzyme, indoleamine-2,3-dioxygenase (IDO). Moreover, SARS-CoV-2 infection can lead to an inflammatory response that affects the levels of some intracellular glycoproteins, such as the intercellular cell adhesion molecule-1 (ICAM-1) and the vascular cell adhesion protein-1 (VCAM-1). A decrease in IDO during pathogenic infections leads to an increase in VCAM-1 in endothelial cells of vessel walls.
About the study
In the present study, researchers collected and analyzed serum samples from 150 patients, 44 of whom tested positive for COVID-19 but exhibited mild disease. They determined whether the neurotoxic metabolites and glycoproteins involved in inflammation were altered in these patients.
A recent study showed that the inflammatory response to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), driven by monocyte-derived macrophages, was detectable in convalescent COVID-19 patients following mild infection. ICAM-1 and VCAM-1 are also involved in the inflammatory response governing immune cell migration to the sites of T-cell-mediated immunity in tissues. Therefore, the authors also determined whether the ICAM-1 and VCAM-1 levels were altered in patients with mild COVID-19 and linked to kynurenine pathway activation.
They used reverse-phase ultra-high-performance liquid chromatography (UHPLC) coupled to a mass spectrometer to quantify all kynurenine pathway metabolites.
Study findings
The researchers found the ICAM-1 and VCAM-1 blood levels were significantly increased in patients with mild SARS-CoV-2, especially those with hypertension. This finding links the increase in endothelial cell adhesion molecules to kynurenine pathway metabolites, such as IDO.
Further, the authors observed a higher KYN/TRP ratio in SARS-CoV-2-positive patients compared to the healthy controls and those testing SARS-CoV-2-negative. Along with a higher KYN/TRP ratio, hypertensive COVID-19 patients had a higher cerebrospinal fluid (CSF) QUIN/TRP ratio. The KYN/TRP ratio is an indirect measure of the IDO activity, whereas the QUIN/TRP ratio is an early, predictive marker of a central nervous system (CNS) disease.
The authors did not observe any differences in serum IFN-ɣ levels in samples from COVID-19 patients with mild disease. In addition to IFN-ɣ, some non-canonical pathways might activate IDO. It explains the activation of the kynurenine pathway observed in the current study cohort. The kynurenine pathway activation leads to long-lasting inflammation; thus, kynurenine metabolites could be potent diagnostic markers for long COVID patients.
Cihan and colleagues analyzed kynurenine pathway metabolites and inflammatory cytokines to find a positive correlation between interleukin-6 (IL-6) and its various metabolites. The present study also found a positive correlation between IL-6 and 3-HK, as well as between IL-6 and QUIN. Furthermore, QUIN, 3-HK, and KYN increased in patients with mild COVID-19. Therefore, the inflammation observed in COVID-19 patients could be a major contributor to the neuronal damage caused by neurotoxic metabolites.
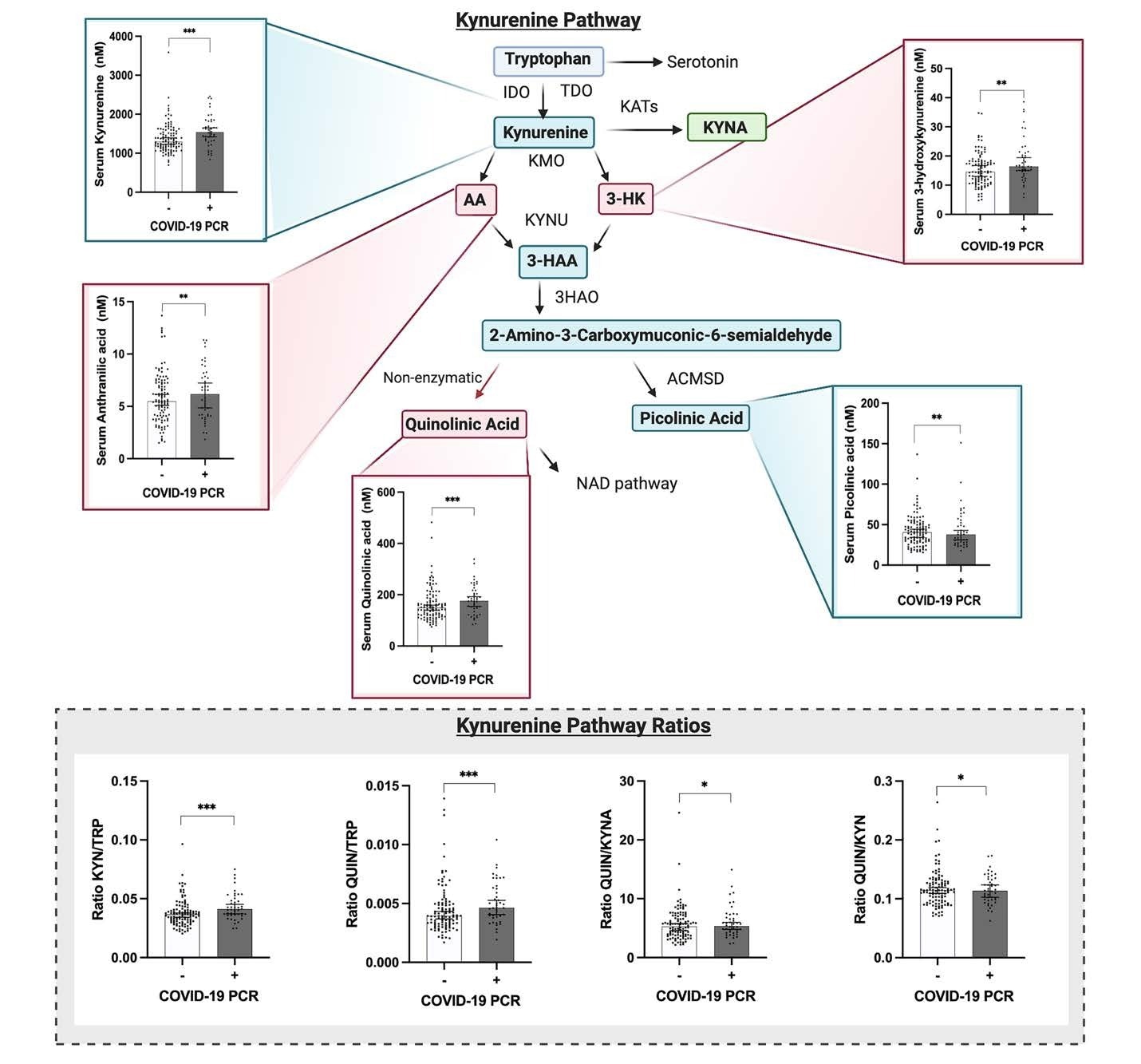 The kynurenine pathway is altered in patients with mild COVID-19, who present increased levels of neurotoxic metabolites. Significantly increased levels of kynurenine (data adjusted for age and sex, ANOVA test F: 11.195, p<0.001 ***), 3-hydroxykynurenine (data adjusted for age and sex, ANOVA test F: 3.390, p=0.009 **), anthranilic acid (data adjusted for age and sex, ANOVA test F: 4.024, p=0.009 **), and quinolinic acid (data adjusted for age and sex, ANOVA test F: 8.492, p<0.001 ***) were found in patients with mild COVID-19 when compared to controls. When the ratio of the metabolites was analyzed, significantly increased levels of KYN/TRP (data adjusted for age and sex, ANOVA test F: 6.377, p<0.001 ***) and QUIN/TRP (data adjusted for age and sex, ANOVA test F: 5.837, p<0.001 ***), as well as QUIN/KYNA (data adjusted for age and sex, ANOVA test F: 2.847, p= 0.040 *) were found in patients with COVID-19. Graphs show the median with 95% of CI. Abbreviations: IDO, Indoleamine 2,3-dioxygenase; TDO, Tryptophan 2,3-dioxygenase; KATs, Kynurenine aminotransferase; KYNA, kynurenic acid; KMO, Kynurenine 3-monooxygenase; AA, anthranilic acid; 3-HK, 3-hydroxykynurenine; KYNU, Kynureninase; 3-HAA, 3-hydroxyanthranilic acid; 3HAO, 3-hydroxyanthranilate oxidase; ACMSD, Aminocarboxymuconate-semialdehyde decarboxylase, and NAD, Nicotinamide adenine dinucleotide.
The kynurenine pathway is altered in patients with mild COVID-19, who present increased levels of neurotoxic metabolites. Significantly increased levels of kynurenine (data adjusted for age and sex, ANOVA test F: 11.195, p<0.001 ***), 3-hydroxykynurenine (data adjusted for age and sex, ANOVA test F: 3.390, p=0.009 **), anthranilic acid (data adjusted for age and sex, ANOVA test F: 4.024, p=0.009 **), and quinolinic acid (data adjusted for age and sex, ANOVA test F: 8.492, p<0.001 ***) were found in patients with mild COVID-19 when compared to controls. When the ratio of the metabolites was analyzed, significantly increased levels of KYN/TRP (data adjusted for age and sex, ANOVA test F: 6.377, p<0.001 ***) and QUIN/TRP (data adjusted for age and sex, ANOVA test F: 5.837, p<0.001 ***), as well as QUIN/KYNA (data adjusted for age and sex, ANOVA test F: 2.847, p= 0.040 *) were found in patients with COVID-19. Graphs show the median with 95% of CI. Abbreviations: IDO, Indoleamine 2,3-dioxygenase; TDO, Tryptophan 2,3-dioxygenase; KATs, Kynurenine aminotransferase; KYNA, kynurenic acid; KMO, Kynurenine 3-monooxygenase; AA, anthranilic acid; 3-HK, 3-hydroxykynurenine; KYNU, Kynureninase; 3-HAA, 3-hydroxyanthranilic acid; 3HAO, 3-hydroxyanthranilate oxidase; ACMSD, Aminocarboxymuconate-semialdehyde decarboxylase, and NAD, Nicotinamide adenine dinucleotide.
Conclusions
To summarize, the study results demonstrated an increase in blood levels of neurotoxic metabolites of the kynurenine pathway in patients with mild COVID-19. These neurotoxic metabolites correlated with inflammatory and vascular injury markers, such as VCAM-1, tumor necrosis factor (TNF)-α, IL-6, and ICAM-1. Future studies should further evaluate their potential as biomarkers for long COVID and as potential contributors to the underlying mechanisms of long COVID.

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Journal reference:
- Preliminary scientific report.
Increased levels of circulating neurotoxic metabolites in patients with mild Covid19, Estibaliz Santiago-Mujika, Kevin Heinrich, Sonia George, Colt D Capan, Cameron Forton, Zachary Madaj, Amanda R Burmeister, Matthew Sims, Andrew Pospisilik, Patrik Brundin, Stewart F Graham, Lena Brundin, bioRxiv pre-print 2022, DOI: https://doi.org/10.1101/2022.06.22.497189, https://www.biorxiv.org/content/10.1101/2022.06.22.497189v1