By 2021, around 82.5% of the United Kingdom (UK) population had received a two-dose regimen of COVID-19 vaccines. However, there is no information about the uptake of COVID-19 vaccination for the nine million UK population stratified by BMI groups.
Studies have shown that the effectiveness of the influenza vaccine is lower among individuals with a higher BMI. Since COVID-19 is also a respiratory infection; therefore, it warrants investigation of whether there is an association between BMI and COVID-19 vaccine effectiveness (VE). In addition, the long-term evidence across a range of COVID-19 outcomes in all BMI groups is also needed because it might reveal the need for alternative risk mitigation strategies and targeted vaccine booster programs for people at high risk.
About the study
In the present observational cohort study, researchers used the QResearch database of general practice records to identify individuals for whom the BMI data was available and who were vaccinated between December 8, 2020, and November 17, 2021, in England. They calculated vaccine uptake as the fraction of individuals with zero, one, two, or three vaccine doses across four BMI categories. The BMI categories were - underweight (<18.5kg/m2), healthy weight (18.5 to 24.9kg/ m2), overweight (25 to 29kg/ m2) , and obese (>30kg/ m2). The study analysis accounted for several demographic confounders, including age, sex, ethnicity, socioeconomic status, and relevant comorbidities.
The team also investigated VE against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Further, using a matched case-control design, they estimated the odds ratio (OR) for severe COVID-19 outcomes in vaccinated individuals vis-à-vis those who had not, considering vaccine dosage and time elapsed since vaccination. Lastly, they estimated the risk of severe COVID-19 outcomes associated with BMI following vaccination using multivariable cox proportional hazard models.
Study findings
Of 9,171,524 participants, 5,666,461 were COVID-19 positive during the study duration. Eventually, 32,808 COVID-19 positive participants were hospitalized, and 14,389 died. Of all the study participants, 19.2% were unvaccinated. Of the remaining participants, 3.1%, 52.6%, and 25% received one, two, and three vaccine dose(s), respectively. The average age of the study participants was 52 years, and the average BMI was 26.7 kg/m².
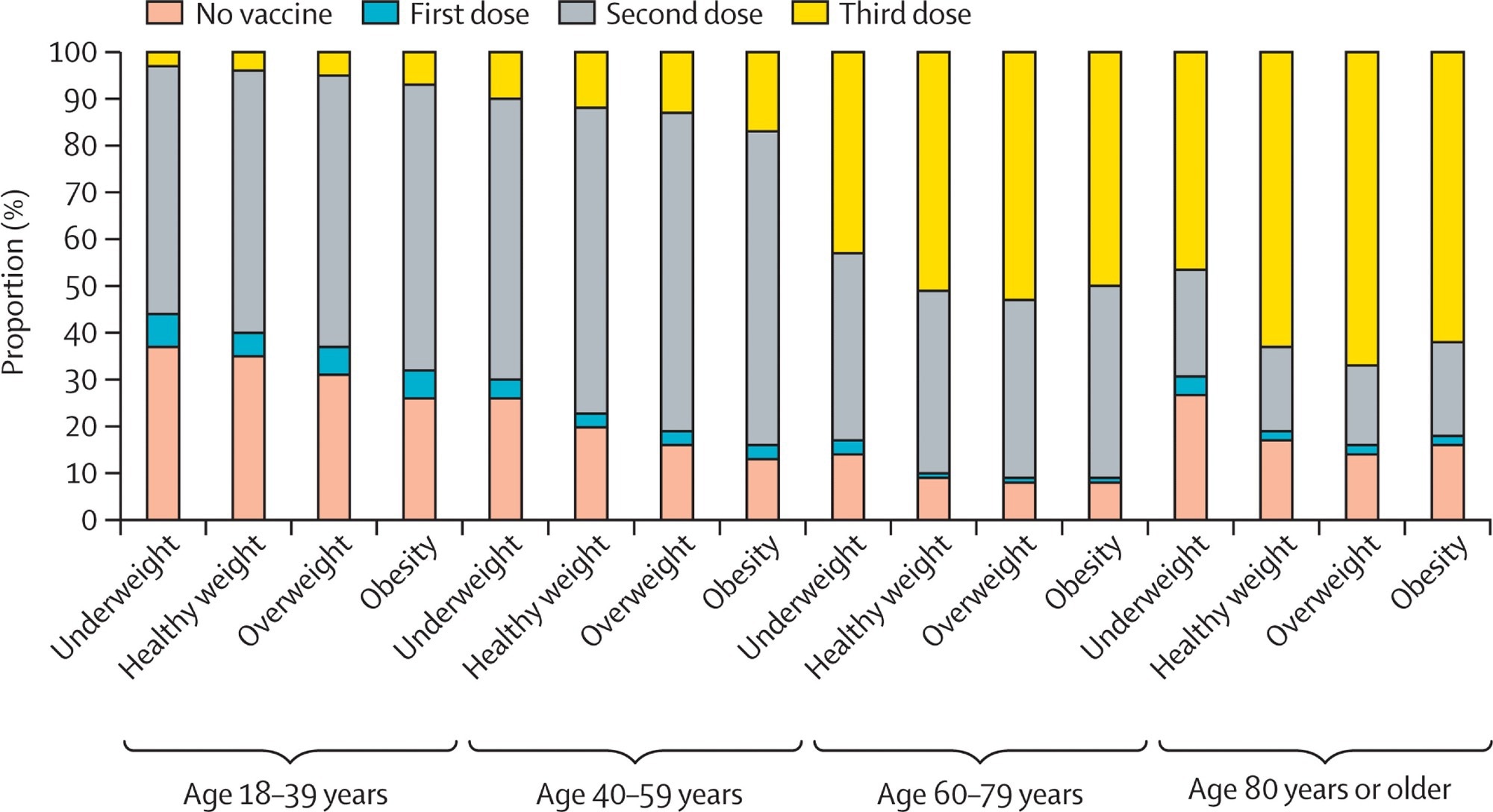 Proportion of people who received no, one, two, or three vaccination doses by age and BMI group
Proportion of people who received no, one, two, or three vaccination doses by age and BMI group
The vaccine uptake was lower in underweight people compared to overweight or obese people (70 to 83% vs. over 80%). These individuals were 40 years or older and had received two or three vaccine doses. Across all four BMI groups, the study results were significantly heterogeneous concerning protection against severe COVID-19.
Accordingly, hospitalization ORs for underweight, normal-weight, overweight, and obese were 0.51, 0.34, 0.32, and 0.32, respectively. Likewise, ORs of COVID-19-related death for under-weight, normal-weight, overweight, and obese were 0.60, 0.39, 0.30, and 0.26, respectively. Compared to unvaccinated individuals, hospitalization and death were higher after 14 days of the second vaccine dose in vaccinated individuals. Also, in the vaccinated participants, the correlation between BMI and COVID-19 hospitalization and death was linear after the first and J-shaped after the second vaccine dose. The researchers observed an inverse U-shaped association between BMI and the third vaccine dose, indicating that a booster was needed to confer complete protection in obese people.
Furthermore, the first and second sets of sensitivity analyses used two different cohorts. The first set had individuals for whom the BMI records for two years before cohort enrollment were available. Their VE showed smaller ORs compared with the primary study analysis; however, the results of both sensitivity analyses were generally in agreement with the main study findings.
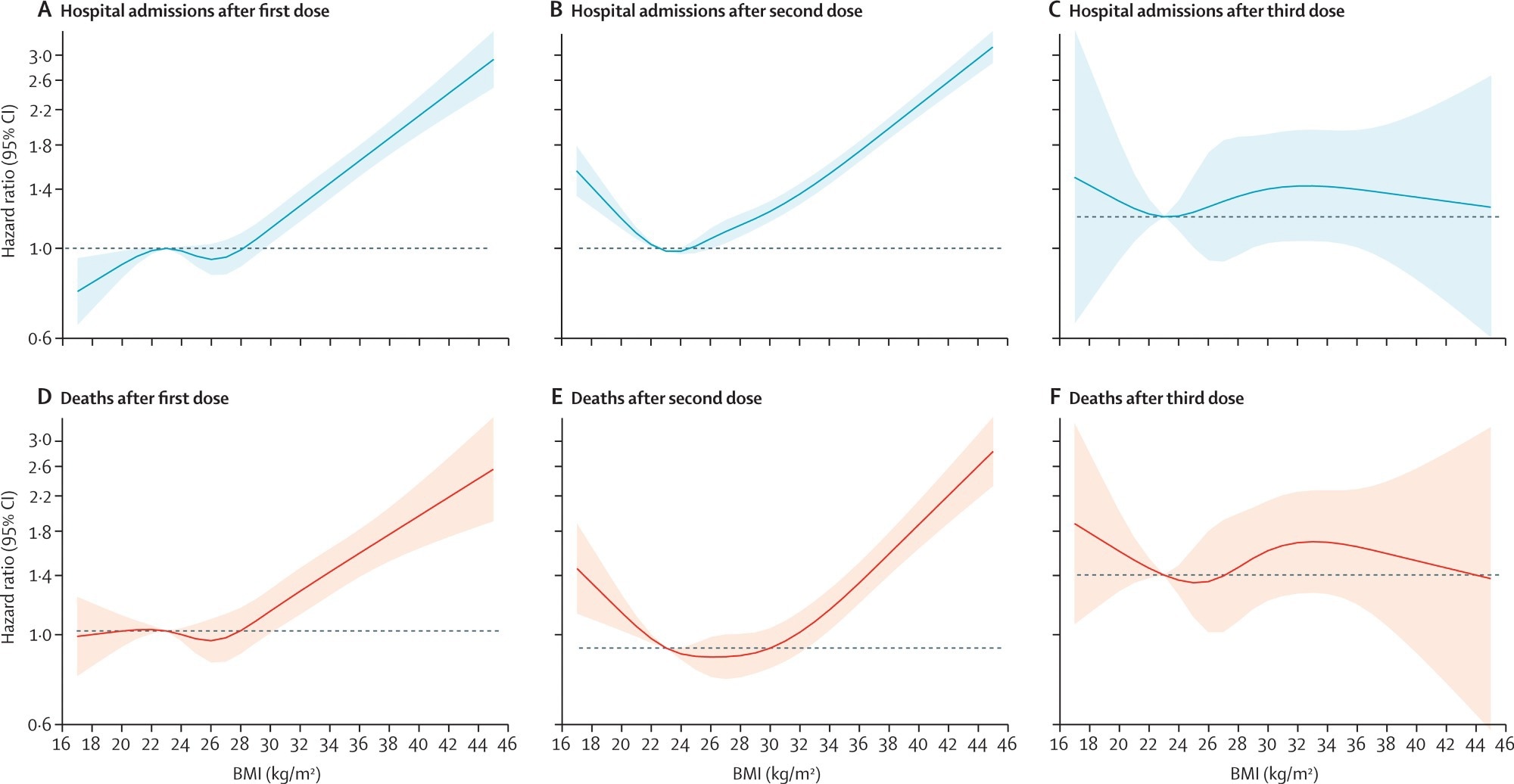 Risk of severe outcomes from COVID-19 after vaccination Estimates of risk after 14 days from each vaccine dose. Adjusted for age, calendar week, sex, ethnicity, socioeconomic status, region, smoking status, hypertension, type 1 diabetes, type 2 diabetes, cardiovascular disease, and care home status. Hospital admissions from COVID-19 after first dose (A), second dose (B), and third dose (C), and deaths from COVID-19 after first dose (D), second dose (E), and third dose (F).
Risk of severe outcomes from COVID-19 after vaccination Estimates of risk after 14 days from each vaccine dose. Adjusted for age, calendar week, sex, ethnicity, socioeconomic status, region, smoking status, hypertension, type 1 diabetes, type 2 diabetes, cardiovascular disease, and care home status. Hospital admissions from COVID-19 after first dose (A), second dose (B), and third dose (C), and deaths from COVID-19 after first dose (D), second dose (E), and third dose (F).
Conclusions
The current large population-based cohort study evidenced that COVID-19 vaccines confer protection against severe disease; however, of similar magnitude in obese as well as normal-weight people. However, the VE had reduced for underweight individuals among those with lower vaccine uptake across all ages. Moreover, the study findings pointed to a higher risk of developing severe COVID-19 in obese and underweight people in the vaccinated cohort because they had lower vaccine uptake and showed much reduced VE. Overall, these results highlighted the need for concerted efforts to increase vaccine uptake in people with BMI less than 18.5 kg/m2. Indeed, creating awareness among people to maintain a healthy weight could help lessen the COVID-19 burden.
Journal reference:
- Associations of BMI with COVID-19 vaccine uptake, vaccine effectiveness, and risk of severe COVID-19 outcomes after vaccination in England: a population-based cohort study, Carmen Piernas, Martina Patone, Nerys M Astbury, Min Gao, Aziz Sheikh, Kamlesh Khunti, Manu Shankar-Hari, Sharon Dixon, Carol Coupland, Paul Aveyard, Julia Hippisley-Cox, Susan A Jebb, The Lancet 2022, DOI: https://doi.org/10.1016/S2213-8587(22)00158-9, https://www.thelancet.com/journals/landia/article/PIIS2213-8587(22)00158-9/fulltext