The coronavirus disease 2019 (COVID-19) pandemic has had a significant impact on global businesses, educational systems, and travel. With a mortality rate of greater than 1% and up to 15% of cases becoming seriously sick, the vast number of COVID-19 cases has overwhelmed healthcare systems in many countries around the world.
The neurological impact of COVID-19 was recognized early on in the pandemic, with post-mortem examination of critically ill patients demonstrating signs of vascular injury in the brain. However, the exact mode of injury remains unclear.
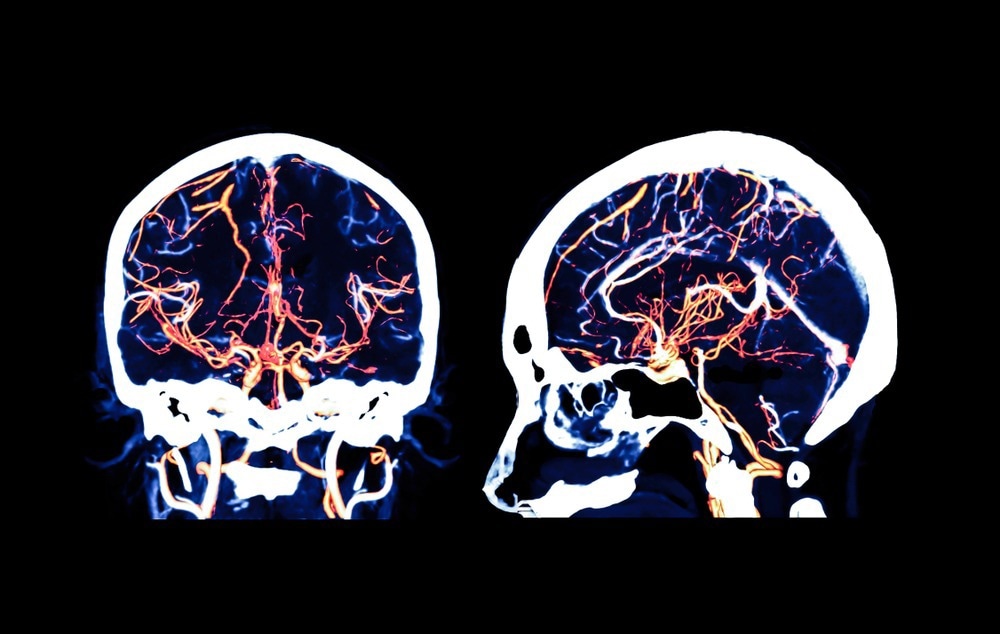 Study: How COVID-19 affects microvessels in the brain. Image Credit: Radiological imaging / Shutterstock.com
Study: How COVID-19 affects microvessels in the brain. Image Credit: Radiological imaging / Shutterstock.com
A recent Brain study discusses the effects of COVID-19 on the brain microvascular system.
Endothelial activation and blood-brain barrier
In the current study, an expert commentary on the description of neurovascular injury, inflammation, and complement activation in the brain is provided. Herein, the authors describe a steep rise in extravasated serum proteins, especially fibrinogen, which indicates a leak in the blood-brain barrier (BBB).
Another important finding was the accumulation of platelets in the brain tissue and upregulation of platelet endothelial cell adhesion molecule 1 (PECAM-1). Other factors that activate the coagulation system are also increased.
This suggests that endothelial activation occurs within the brain’s blood vessels, thereby blocking and damaging the microvessels. This theory is corroborated by earlier results reported by the same authors, wherein they report injured brain blood vessels on post-mortem samples, as well as other studies that show this type of injury on magnetic resonance imaging (MRI) results.
The presence of immune complexes at the vascular wall containing immunoglobulin G (IgG) and IgM, along with complement factors, suggests complement activation has occurred in the brain. This adds to earlier findings of complement activation in COVID-19.
The activated complement factor C5b-9 forms a membrane attack complex (MAC), which is compatible with endothelial cell death. Both endothelial activation and a leaky BBB allow immune cells to enter cells, as demonstrated by the presence of CD3- and CD8+ T-cells, as well as CD68+ macrophages.
Interestingly, these infiltrates are found only around the blood vessels and not the brain itself, thereby indicating that COVID-19 causes indirect neuronal and glial injury. The hindbrain exhibits the greatest impact, perhaps because its vessels are more sensitive to injury or because viral entry is easiest in this region.
Neuronophagia was also observed, thus indicating that some neurons died and were consumed by microglia.
Transcriptomics data were obtained from this region and added to current knowledge about brain involvement in COVID-19. To this end, it appears that in COVID-19, the genes that encode permeability regulating factors like endothelial nitric oxide synthase (eNOS) show different levels of expression than in control patients.
Vascular injury in the brain
Previously, the researchers had proposed that endothelial activation was due to complement activation through the classical pathway in response to immune complexes. This subsequently caused the BBB to become permeable to immune cells.
Other studies have similarly demonstrated the presence of autoantibodies to vascular antigens, which are occasionally capable of activating the endothelium, in the blood and cerebrospinal fluid of patients with severe COVID-19 and long-COVID.
Other sources of endothelial activation could be certain cytokines like tumor necrosis factor (TNF) or interleukins that are found at high levels during the ‘cytokine storm’ observed in severe COVID-19. These cytokines are known to cause endothelial cells to adhere to the blood cells, thereby causing the BBB to become leaky.
Another potential explanation for the vascular injury observed in the brains of COVID-19 patients is the direct effect of viral invasion of the endothelial cells. This has been corroborated by previous studies reporting the presence of viral particles in the brain tissue and vascular cells of these patients.
The induction of apoptosis in infected lung macrophages following infection reduces the rate of viral replication in infected cells and is mediated by the formation of inflammasomes and subsequently followed by hyper-inflammation that arises due to the resulting cytokine storm. This might also occur in the brain and could account for the permeability of the BBB.
Conclusions
The current study shows the importance of understanding the pathophysiology of organ dysfunction in COVID-19, which could cause both acute and post-COVID symptoms. For example, the activation of neuronal glial cells might initiate chronic neurological symptoms, which could be mitigated by therapeutics that are specific to the vascular effects of the infection.
The study by Lee and colleagues is another hint that SARS-CoV-2 infection impairs vascular function, and provides valuable insights into the molecular players involved in the interaction between the vasculature and the immune system.”