As the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus responsible for the coronavirus disease 2019 (COVID-19), has continued to infect millions throughout the world, increasing complaints of chronic symptoms have been reported among those who recover from this disease.
Eventually, these symptoms were recognized as a condition known as ‘long Covid,’ post-acute sequelae of COVID-19 (PASC), or post-covid condition. A new study under review in the journal Scientific Reports and currently available on the Research Square* preprint server suggests that these complaints may not be extremely common among COVID-19 patients as compared to the general population.

Study: Development of Long-Covid, Or Prevalent Complaints in General? Image Credit: Kateryna Onyshchuk / Shutterstock.com

 *Important notice: Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Introduction
PASC causes a wide range of symptoms linked to many organs and is associated with varying severity. Little remains known about this condition, its prevalence, risk factors, and prognosis.
Shortness of breath, cough, brain fog, loss of concentration, and fatigue are the major complaints of PASC. Neurological symptoms also include prolonged alterations in smell and taste. Previous studies published in several different countries have found that some of these symptoms were more common in individuals who had recovered from COVID-19.
The overlap between various complaints often associated with PASC and their development over time in most patients with mild COVID-19 has been debated. Since the vast majority of COVID-19 patients will experience mild symptoms and do not require hospitalization, the need to identify the risk of PASC in this group is evident, especially since mild breakthrough infections are common among vaccinated individuals.
About the study
The current study aims to understand whether PASC really exists and how it changes over time. In addition, the researchers from the Norwegian Institute of Public Health and Lund University examined how similar symptoms evolve over time in non-COVID-19 patients.
Neurological, pulmonary, and general complaints were the primary focus of this study, as these are the most common features reported by PASC patients.
The data used in the current study was acquired from the Norwegian Emergency Preparedness Register of tests for COVID-19 in Norway from the onset of the pandemic and excluded hospitalized patients. This also provided vaccination and demographic data.
All participants were 18-70 years old and were classified as having been tested or not for COVID-19 between August 1, 2020, to August 1, 2021. No participant had a diagnostic code for any of the included PASC complaints six months before the COVID-19 test until the start of the testing week if testing was done.
This allowed for complaints or consultations related to the test rather than for those which predated the test or those that formed part of other tests ordered before a specialist consultation.
Patients were classified as those positive for COVID-19, those who tested negative, and untested persons.
Study findings
Over 76,000 people tested positive for COVID-19, while over 1.1 million were negative and over one million were not tested. Of those who tested positive for COVID-19, 0.05% died, and 0.2% moved out of the area. Of those who were negative, 0.06% died, and 0.1% emigrated to Norway.
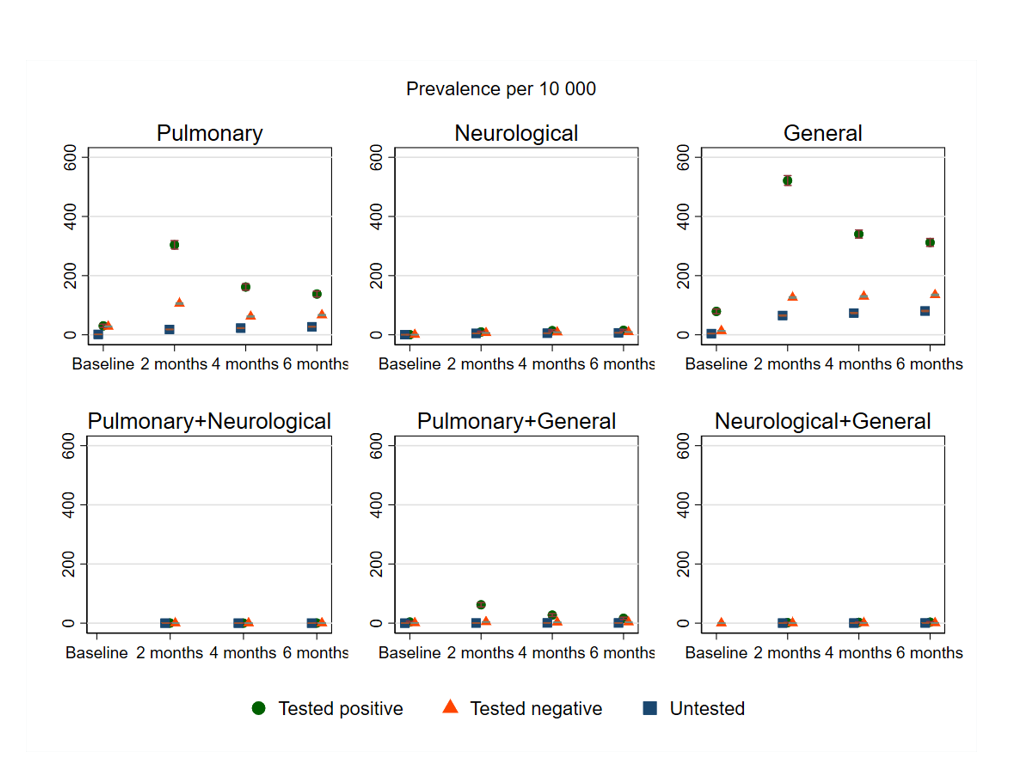
The adjusted prevalence in percent and 95% confidence interval for different post-covid complaints at baseline, 2, 4 and 6 months follow-up for persons testing negative and positive for SARS-CoV-2. Missing circles, triangles or squares indicate no observation for the group in question. The prevalence of pulmonary+neurological+general complaints could not be plotted due to very few observations.
Individuals who tested positive for COVID-19 were more likely to be younger and healthier and were unvaccinated more often than the other two groups. These individuals also had a higher number of medical consultations for general illnesses between 2017-19; however, this increased rate of hospital visits was not reflected when neurological, lung and general complaints were assessed.
The prevalence of single complaints increased over two months from the baseline. However, when lung and general complaints occurred together, their prevalence was reduced between two to six months. Neurological complaints were lower at baseline and increased at a slower rate.
Lung and general complaints were more common in individuals who recovered from COVID-19 than in the other two groups, especially two months after their initial diagnosis. This difference declined at four and six months. The differences between groups were least for neurological complaints and showed no or small differences over time at up to six months from the test date.
At this last time point, 50-250 more people per 10,000 COVID-19 patients might be diagnosed with lung or general complaints as compared to those who were not diagnosed with COVID-19. The difference for neurological complaints was only five to ten people per 10,000. If untested people were excluded, the direct comparison differences were lower.
Overlapping complaints were uncommon in the COVID-19 group, though their complaints were overall higher.
Implications
The study findings indicate a small rise in the prevalence of PASC-like complaints after recovery from COVID-19 from 5-250 per 10,000 people as compared to those who tested negative or the untested population. Most of these complaints occurred either with regard to breathing, fatigue, or neurological symptoms in isolation rather than as a syndrome.
Thus, complaints that are often regarded as typical post-covid complaints may also be naturally prevalent complaints, irrespective of initial disease.”
Even with a small rise in the frequency of such complaints following COVID-19, the burden on the healthcare system may be high because of the sheer magnitude of COVID-19 cases.
When combined with earlier studies, the study findings may indicate that both mild COVID-19 and severe influenza predispose a small rise in lung-related symptoms and fatigue six months after infection in these patients. Nevertheless, the World Health Organization (WHO) has defined PASC as very rare as a result of its low prevalence.
Further research that is based on more sensitive patient reports or clinical data will be required to validate these findings and determine how other mild viral respiratory infections correlate in terms of long-term sequelae. The impact of booster vaccination doses on PASC, as well as risk factors for post-covid complaints, remains to be established.

 *Important notice: Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.