
 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Background
Throughout the world, cardiovascular diseases remain the leading cause of death among men and women. Although COVID-19 primarily affects the respiratory system, it is also associated with several non-pulmonary consequences, including effects on the cardiovascular system.
Although rare, COVID-19 vaccines have been associated with cardiovascular manifestations. For example, the Pfizer-BioNTech messenger ribonucleic acid (mRNA)-based COVID-19 BNT162b2 vaccine was found to induce myocarditis in some individuals, whereas vector-based vaccine caused thrombotic thrombocytopenia in rare instances.
In France, cardiovascular diseases were the second most common cause of hospitalization in 2019. After the initial detection of COVID-19 in January 2020, France faced a shortage of healthcare management services. Three lockdowns were subsequently implemented between March 2020 to May 2021 to reduce the transmission of COVID-19 and the burden on healthcare services.
About the study
The current retrospective cohort study analyzed variations in the incidence of cardiovascular diseases pre- and post-COVID-19 in France. This analysis also considered the ways in which COVID-19 vaccination may have altered incident case rates.
The French National Uniform Hospital Data Set Database (PMSI) provided data from 2019-2021, with 2019 considered as the reference year. COVID-19 vaccination data were acquired from the French Ministry of Solidarity and Healthcare web portal.
International Statistical Classification of Diseases and related health problems, 10th revision (ICD10) codes were used to identify cardiovascular pathologies, with a primary focus on inflammatory and thromboembolic processes. These diseases were divided into five categories, which included:
- Group I: “Heart-Ischemic,” which included myocardial infarction (MI) and angina pectoris
- Group II: “Heart- Inflammation,” which included myocarditis and pericarditis
- Group III: “Cerebrovascular,” which included transient ischemic attack (TIA) or stroke
- Group IV: “Arterial embolism and thrombosis”
- Group V: “Venous embolism and thrombosis,” which included deep vein thrombosis (DVT), PE, and other venous thromboses
For each pathology, only cases that were hospitalized for the first time in two years between 2019 and 2021 were included.
Study findings
A total of 919,514 patients were studied for ten pathologies. A significant decline in hospitalizations was observed for all pathological conditions preceding the first lockdown between March 2020 and April 2020.
During this period, the rate of angina pectoris and arterial thrombosis/embolism declined by more than 35%, whereas a decline of about 30% was observed for patients with DVT. MI, TIA, and myocarditis rates also declined by 20-23%, whereas the incidence of pericarditis- and stroke-related hospitalizations declined by 13% and 14%, respectively. PE hospitalizations declined by 4%.
Four pathological groups with similar temporal patterns were identified based on the case ratios between each year, case trend, and annual relative risk. These groups were defined as sustained decrease, attenuated decrease, partial rebound, and increase.
In group A, which was otherwise known as the sustained decrease group, the incidence and relative risk of hospitalizations significantly declined each year and overall. Angina pectoris and DVT cases were included in this group.
In group B, otherwise known as the attenuated decrease group, a significant decrease in hospitalizations was reported by 2020 and was followed by an unchanged rate of hospitalizations between 2020 and 2021. This group included TIA, stroke, other venous thromboses, and pericarditis cases.
In the partial rebound group C, a significant decrease in 2020 cases was followed by a significant increase in hospitalizations in 2021. MI, arterial embolism, and thrombosis hospitalizations were included in this group.
In the increasing group D, PE and myocarditis cases were associated with an increase in their relative risk for hospitalization and overall incidence. These changes were independent of 2019 to 2020 changes.
Further analysis revealed a progressive rise in myocarditis-related hospitalizations from May to August 2020, until ultimately declining between September and October 2021. Notably, myocarditis occurred more frequently in men between the ages of 10 and 19, as well as those between 20 and 29 years of age, in 2021 as compared to 2019.
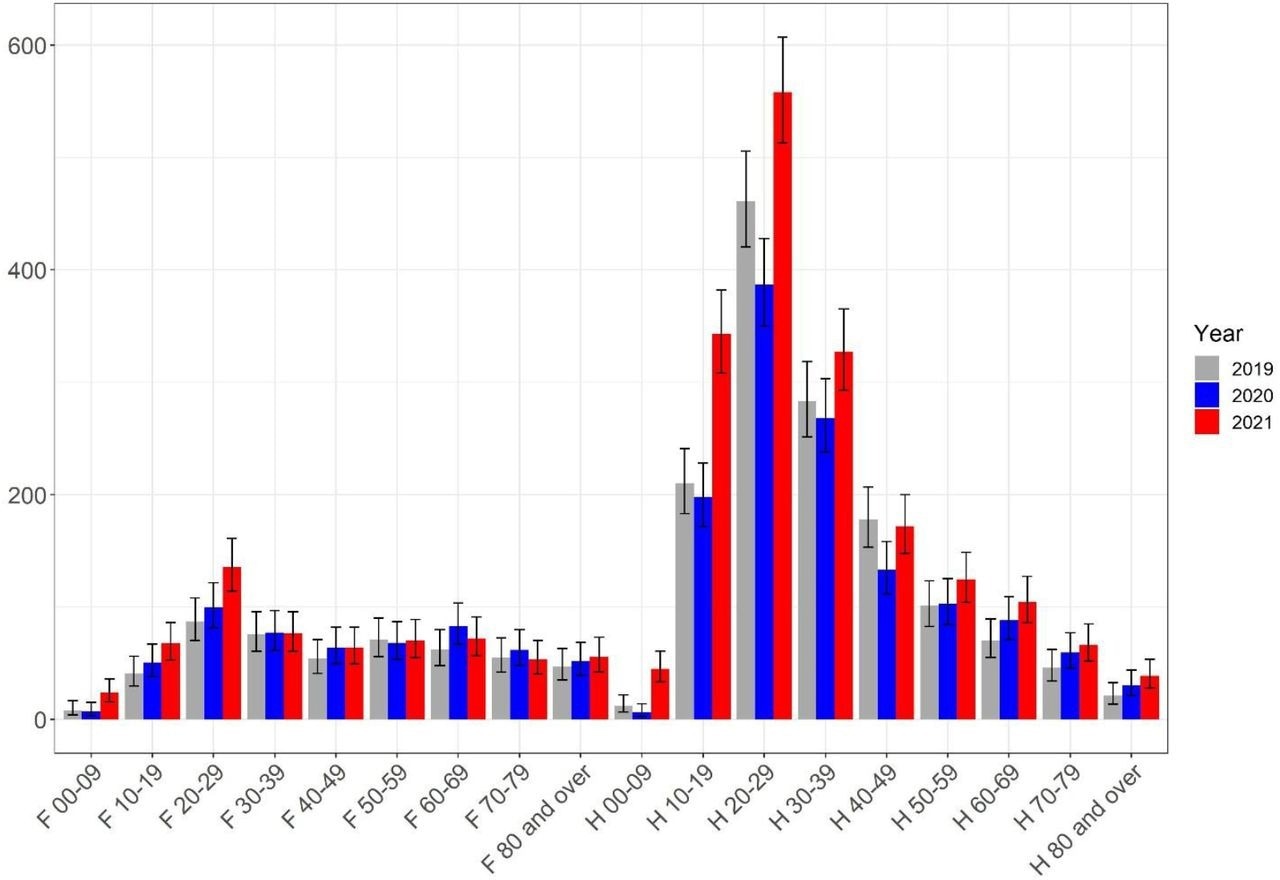 Myocarditis, caseload per sex and age, per year.
Myocarditis, caseload per sex and age, per year.
Conversely, a more even distribution of excess cases was observed in terms of both the age and sex of PE patients. The most notable differences were observed in elderly patients, particularly females over 70 years of age.
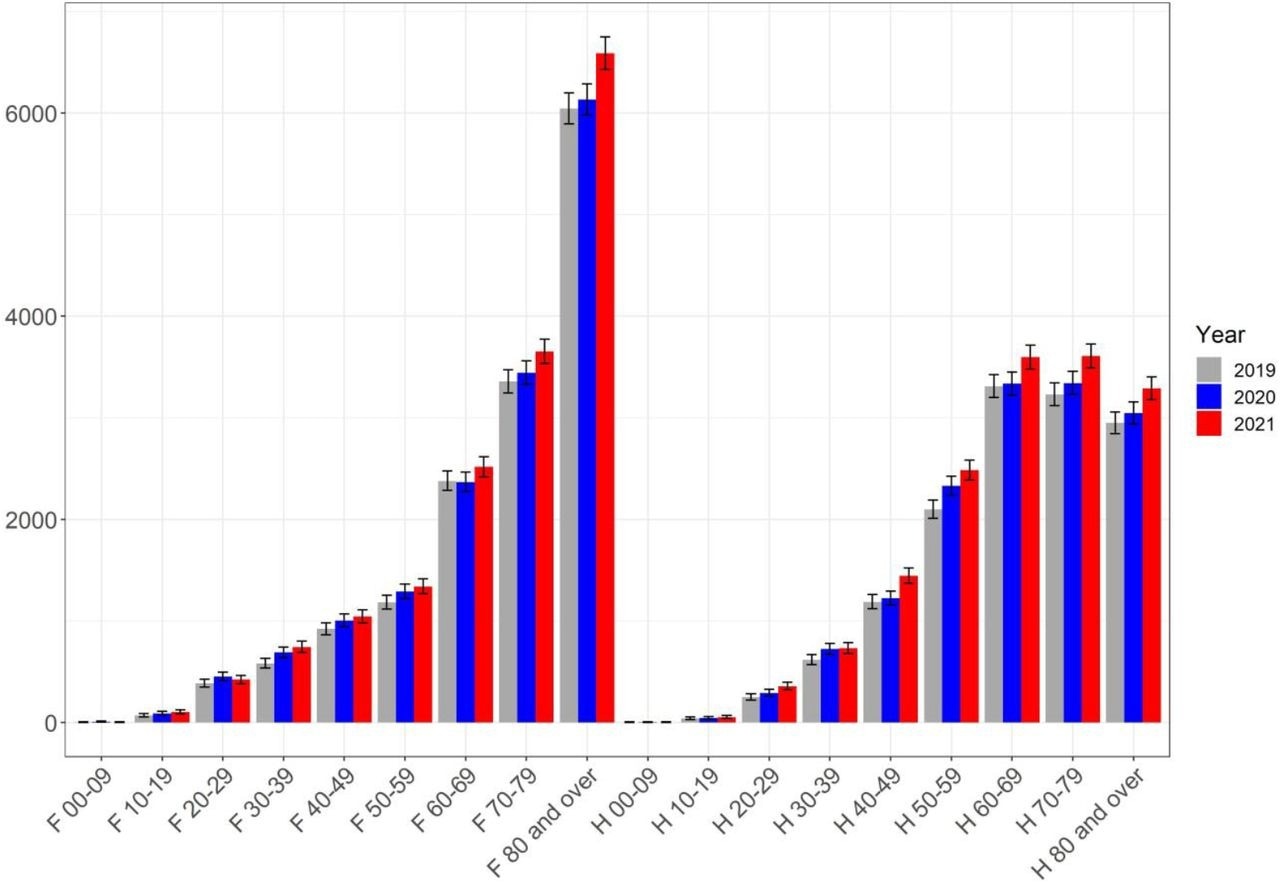 Pulmonary embolism, caseload per sex and age, per year.
Pulmonary embolism, caseload per sex and age, per year.
When vaccination data was considered for non-COVID-19-related hospitalizations, a significant increase in myocarditis hospitalizations was reported among men between 10-29 years of age in March 2020. A similar rise in myocarditis cases was reported between June and October 2021 in this age group, which corresponded to when they were eligible for their first dose of COVID-19 vaccines.
A similar trend was reported among women aged 70 years and older with PE and their first COVID-19 vaccine doses.
Conclusions
Except for PE and myocarditis, all other targeted cardiovascular pathologies were found to decline between January and October 2021 as compared to 2019. These declined admission rates reflect the significant number of patients throughout France who did not have access to hospital services at this point in the pandemic.
The subsequent rise in acute coronary atherothrombosis reported in 2021 may be a re-normalization of necessary hospital care after this period. These findings suggest that the healthcare system in France faced significant challenges in providing important cardiac care to patients in 2021, despite any lessons that they may have learned during the first year of the pandemic.
The rise in myocarditis cases may be attributed to limited access to cardiac care in hospitals, as well as adverse reactions to current COVID-19 vaccines. Similarly, the rise in PE cases also occurred simultaneously when certain patient groups were eligible for their first COVID-19 vaccine doses.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.