The ongoing coronavirus disease 2019 (COVID-19) pandemic, which is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has significantly affected the global healthcare sector and economy. To date, SARS-CoV-2 has infected over 584 million and claimed more than 6.41 million lives worldwide.
Researchers have worked at an unprecedented speed to analyze various aspects of COVID-19 in an effort to design effective pharmaceutical and non-pharmaceutical measures to protect individuals from this disease.
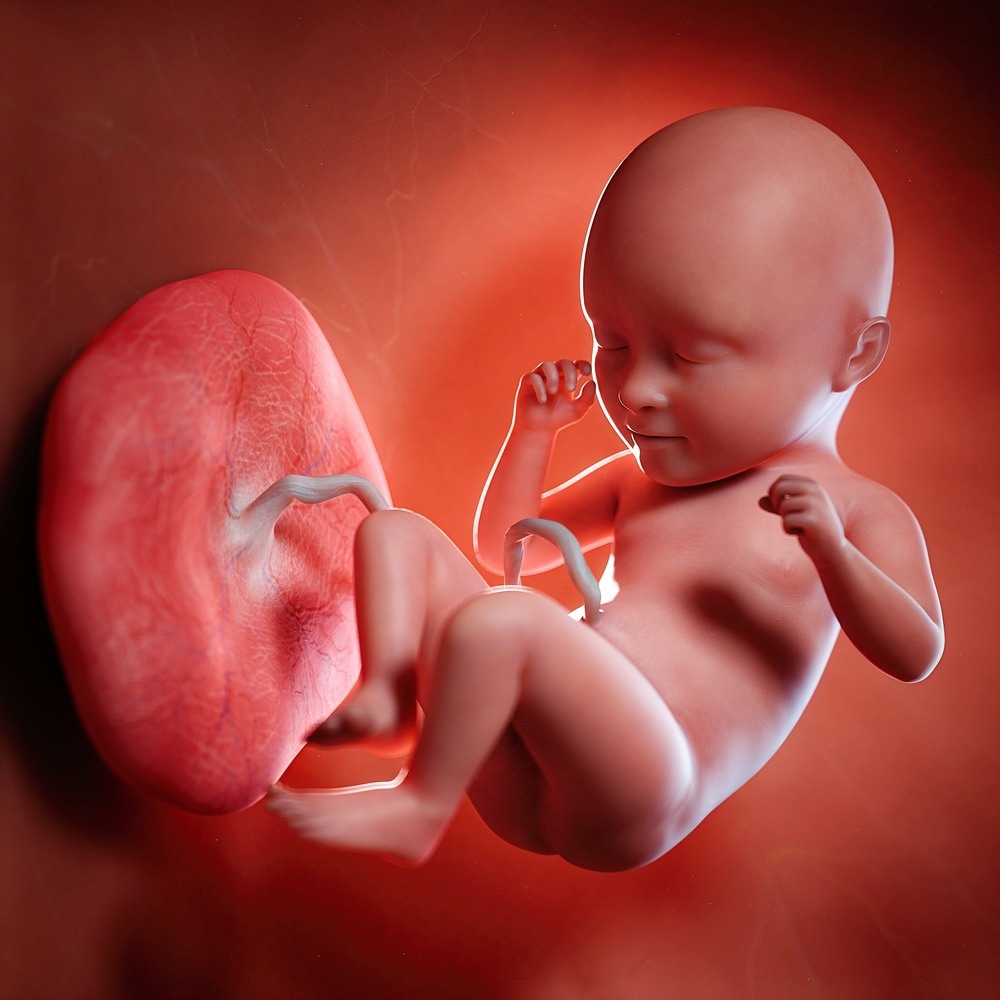
Study: The placental pathology in Coronavirus disease 2019 infected mothers and its impact on pregnancy outcome. Image Credit: SciePro / Shutterstock.com
Background
Pregnancy induces an immunocompromised state in the mother, thereby making her more vulnerable to viral respiratory infections. Previous studies have revealed that the placenta, which provides nutrients to the fetus, exhibits an attenuated immune response and hosts many viral infections.
Some maternal conditions that might affect pregnancy outcomes include inflammatory activation, hypoxia, and increased thrombotic events secondary to COVID-19. Although the placental features in COVID-19 have been described, there remains a lack of evidence regarding the characteristic pathological outcomes associated with placental pathologies resulting from COVID-19.
About the study
In a recent Placenta journal study, researchers describe the impact of placental morphological changes in COVID-19 on pregnancy outcomes.
The current study was conducted at the Postgraduate Institute of Medical Sciences and Research (PGIMER), Chandigarh, India, between July 1, 2020, and June 30, 2021. Pregnant women with COVID-19 who delivered at PGIMER were included in the study.
All pregnant women tested positive for COVID-19 as confirmed by reverse transcription-polymerase chain reaction (RT-PCR) assay or GeneXpert Dx Xpress SARSCoV-2 RT-PCR assay. Only women who delivered at more than 20 weeks of gestation were included in the study cohort.
Relevant data such as demographic characteristics, mode of delivery, COVID-19 severity, obstetrical complications, maternal mortality, and neonatal details of selected candidates were assessed.
Study findings
A total of 179 placentae obtained from 170 participants were analyzed in the current study. Over 49% of placentae exhibited at least one abnormal feature based on histopathological examination (HPE).
More specifically, almost 28% exhibited maternal vascular malformation, which was followed by villous fibrin deposition, fetal vasculopathy, and acute inflammation at rates of about 23%, 17%, and 7%, respectively. These findings are consistent with previous reports that revealed the majority of placental abnormalities were linked with fetal vasculopathy, followed by villitis, intervillositis, and chorioamnionitis.
The presence of placental abnormalities was not related to COVID-19 severity. In contrast to previous studies, the risk of preeclampsia or clinically detected abruptio placentae was not elevated in mothers with abnormal placental pathologies.
Placental morphologic examination revealed an elevated incidence of retroplacental (RP) clots/hemorrhages. This might be due to silent antepartum hemorrhages caused by COVID-19.
Pregnancy outcomes were compared between COVID-19-positive mothers with abnormal placental morphology and COVID-19-positive mothers with normal placental morphology.
To this end, an increased risk of stillbirths was observed in COVID-19 mothers with abnormal placentae. These stillbirths were clinically unexplained, as clinicians did not observe the incidence of pre-eclampsia, fetal growth restriction (FGR), intrahepatic cholestasis of pregnancy (ICP), or abruptio placentae.
Infants born to SARS-CoV-2-infected mothers with abnormal placental morphologic features exhibited significantly lower Apgar scores at one minute and five minutes, which indicates the overall health of a newborn. However, lower Apgar scores did not affect NICU admissions.
Nevertheless, a significant correlation was observed between RP clot/hemorrhage and intervillous fibrin deposition at lower Apgar scores.
A systematic enhancement in thrombotic events and microvascular injury syndrome as a result of COVID-19 might affect the placenta. This could lead to rapid or slow blood flow, decreased fibrinolysis, elevated levels of fibrin degradation products, and increased hypoxic-ischemic injury.
Conclusions
Taken together, 50% of the study participants’ placentae exhibited abnormal morphologic features. Furthermore, pregnant women with COVID-19 and abnormal placental morphologies were associated with poor pregnancy outcomes.
The current study is likely the first to correlate placental morphological features in COVID-19-positive pregnant women with pregnancy outcomes. A key strength of this study is its large cohort.
Nevertheless, one of the key limitations is that the study findings were not compared with non-COVID-19 controls. As a result, the scientists failed to confirm that all placental changes and pregnancy outcomes were solely related to COVID-19 rather than any other factors.
In the future, more research is needed to elucidate the effect of the SARS-CoV-2 burden on the extent of the placental injury.
Journal reference:
- Joshi, B., Chandi, A., Srinvasan, R., et al. (2022). The placental pathology in Coronavirus disease 2019 infected mothers and its impact on pregnancy outcome. Placenta 127(1-7). doi:10.1016/j.placenta.2022.07.009