The first case of monkeypox associated with this outbreak was identified in May 2022 in Massachusetts, United States. Following this, it has been reported in all 50 states, 1 US territory, and the District of Columbia (DC). The transmission of MPXV has been found to occur through close contact with infected people or animals. Infections lead to a febrile illness that further causes vesiculopustular rash and lymphadenopathy.
However, infections in the current Clade II outbreak were found to be different. The febrile illness is primarily absent or mild, and the rash is reported in the oral, anal, or genital regions. Moreover, the occurrence of neuroinvasive disease has been observed to be rare.
A new study published in the CDC's Morbidity and Mortality Weekly Report analyzed two people with encephalomyelitis associated with monkeypox disease in Colorado and DC during the current outbreak.
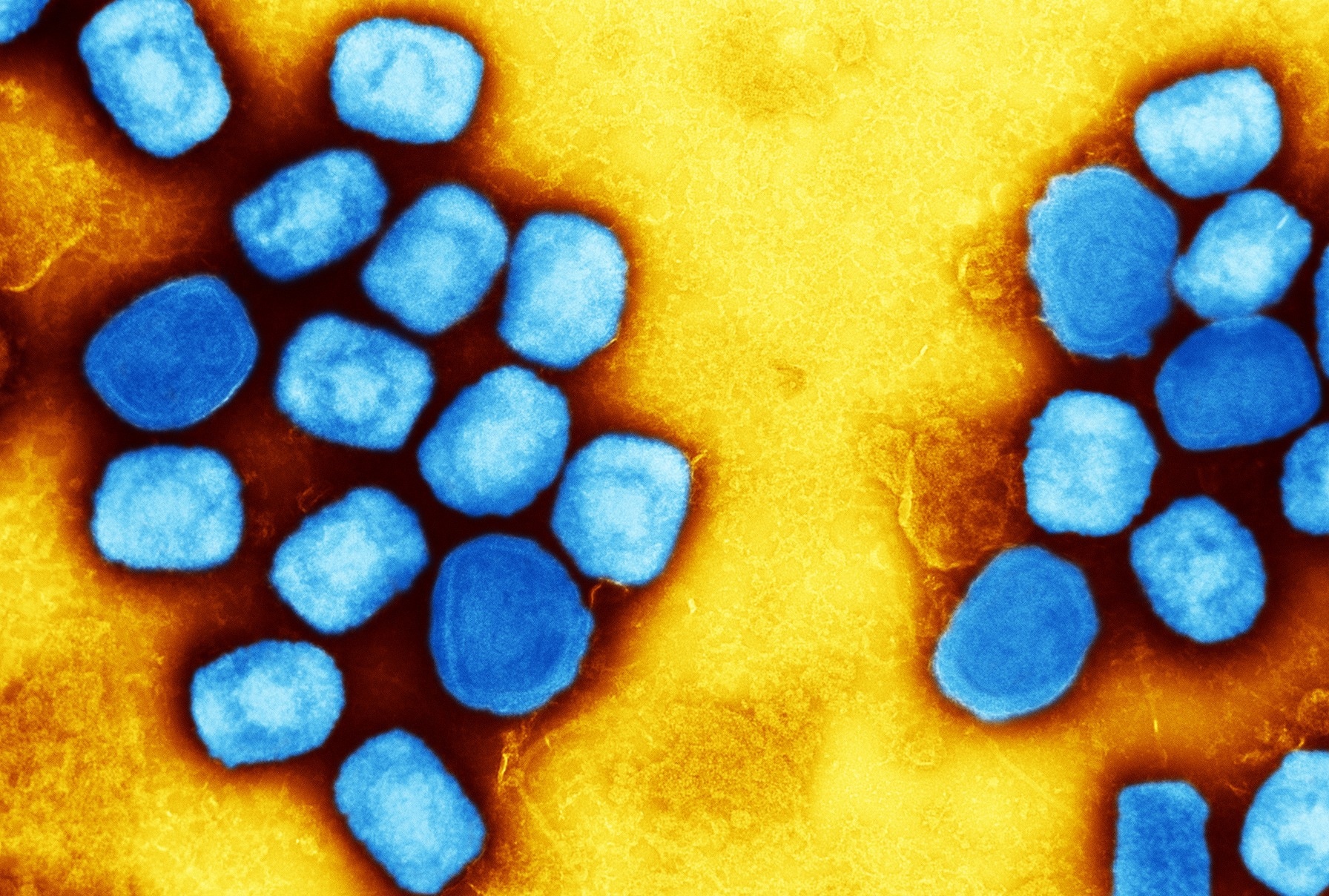 Two Cases of Monkeypox-Associated Encephalomyelitis — Colorado and the District of Columbia, July–August 2022. Image Credit: NIAID
Two Cases of Monkeypox-Associated Encephalomyelitis — Colorado and the District of Columbia, July–August 2022. Image Credit: NIAID
First patient
The first patient was reported to be a healthy, immunocompetent gay man who lived in Colorado and was in his 30s. He described no recent exposure to MPXV or travel, nor was he vaccinated against monkeypox or smallpox. However, he reported the development of chills, fever, and malaise in July 2022. After that, an itchy vesiculopustular rash developed three days post symptom onset on his face, spreading to his scrotum and extremities. Development of weakness and numbness in the left upper and lower extremity, intermittent priapism, and urinary retention were reported nine days after the onset of symptoms, followed by hospitalization.
A positive polymerase chain reaction (PCR) test result was obtained from his swab lesions, confirmed to contain MPXV DNA. Partially enhancing lesions in the frontal lobes, as well as non-enhancing lesions of the bilateral medial thalami, bilateral basal ganglia, pons, and splenium, were observed through magnetic resonance imaging (MRI) of the brain. Multifocal, partially enhancing lesions of the gray matter of the conus medullaris and central thoracic spinal cord were observed through an MRI of the spine.
64 mg/dL of glucose, 155 white blood cells/μL, nine red blood cells/μL, and 273 mg/dL of protein were detected from the cerebrospinal fluid (CSF) analysis. CSF bacterial cultures, along with CSF varicella-zoster virus (VZV) and herpes simplex virus (HSV) PCR results, were found to be negative. Myelin oligodendrocyte glycoprotein (MOG) and serum aquaporin-4 antibody results were also negative. Additionally, results for HIV, CSF, and serum MPXV, as well as SARS-CoV-2, were reported to be negative. Particle agglutination test and serum treponemal antibodies results were positive, while CSF venereal disease research laboratory (VDRL) and serum rapid plasma reagin (RPR) test results were found to be negative.
Oral tecovirimat was administered following the onset of neurologic symptoms. Administration of pulsed intravenous (IV) methylprednisolone, IV penicillin, and IV immunoglobulin (IVIG) led to little improvement in weakness and numbness. However, the patient's progress was found to plateau after two weeks. Plasma exchange (PLEX) was given to overcome this. The resolution of skin lesions took place after three weeks. Finally, he was discharged to outpatient rehabilitation therapy and could walk with an assistive walking device. He was also referred to outpatient neurosurgery due to the narrowing of his spinal cord.
Second patient
The second patient was also reported to be a healthy, immunocompetent gay man who lived in DC and was in his 30s. Like the previous patient, he had no exposure to MPXV, travel history, or vaccination against monkeypox or smallpox. He reported early symptoms of myalgia and fever, followed by the development of vesiculopustular rashes in his trunk, face, extremities, and perianal region. Development of bladder and bowel incontinence, along with weakness of both lower extremities, was reported five days after the onset of symptoms, followed by hospitalization. After that, the next two days observed an altered mental state and reduced consciousness. Following this, he was intubated and shifted to the intensive care unit.
Non-enhancing lesions of the medulla, cerebellum, and pons were observed through an MRI of the brain. Multifocal, partially enhancing lesions in the upper thoracic regions and the central cervical were observed through the MRI of the spine. Pelvic lymphadenopathy and rectal thickening were observed with the help of computed tomography imaging of the pelvis and abdomen. In addition, 60 mg/dL of protein, 65 mg/dL of glucose, 4 red blood cells/μL, and 30 white blood cells/μL were detected by CSF analysis. CSF bacterial cultures, CSF MOG, and aquaporin-4 antibodies, as well as CSF VZV and HSV PCR results, were all found to be negative. However, the presence of 3 CSF-specific oligoclonal bands was reported. Additionally, HIV, urine and rectal gonorrhea, chlamydia, CSF VDRL, RPR as well as SARS-CoV-2 results were reported to be negative.
Administration of oral tecovirimat took place two days after the onset of neurologic symptoms. However, it was replaced by IV tecovirimat due to absorption issues. Pulsed IV methylprednisolone was administered, which led to little improvement in cognition. Administration of IVIG was discontinued due to the development of high fevers by the patient. Following PLEX, improvement in speaking, lower extremity weakness, and following commands were observed. The resolution of skin lesions took place after five weeks. He was given IV rituximab to maintain immunosuppressive therapy. Finally, he was discharged to acute inpatient rehabilitation and could walk using an assistive walking device.
Conclusion
The current study confirmed that both patients had MPXV infections along with encephalomyelitis. There was, however, a lack of understanding of the underlying pathology. It might have been caused due to invasion of the CNS by MPXV or the triggering of an autoimmune process by systemic MPXV infection. However, MPXV nucleic acid was not detected in the CSF. Therefore, public health professionals and clinicians must be aware of the various clinical presentations of MPXV infections and treatment options. Moreover, suspected cases must be reported to territorial, local, state, or tribal health departments to understand symptoms better and develop suitable treatments. Finally, people belonging to high-risk groups, along with those exposed to MPXV infections, must be vaccinated to reduce the spread of the disease.