The coronavirus disease 2019 (COVID-19) pandemic brought about by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has adversely impacted public health worldwide, leading to millions of deaths. Vaccination is considered to be the most effective intervention for the reduction of COVID-19-related severe disease and death.
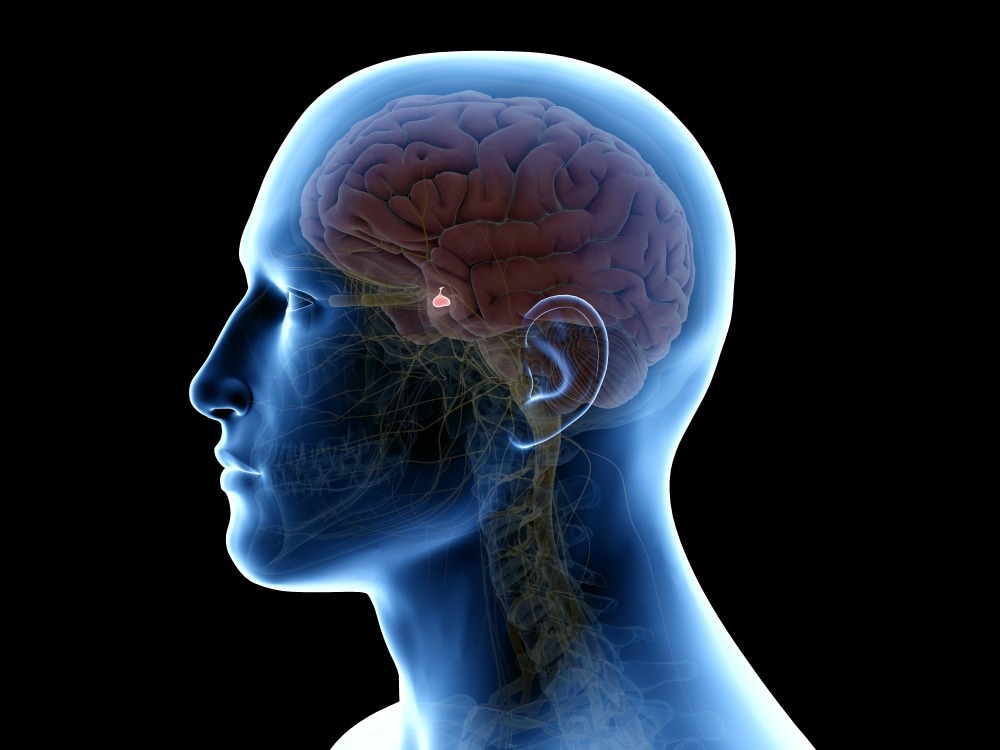 Study: Central diabetes insipidus revealing a hypophysitis induced by SARS-CoV-2 vaccine. Image Credit: SciePro/Shutterstock
Study: Central diabetes insipidus revealing a hypophysitis induced by SARS-CoV-2 vaccine. Image Credit: SciePro/Shutterstock
Background
Systemic and local side effects have been common, especially after the second vaccination. These include headache, malaise, fever, arthralgia, and myalgia. However, these side effects are moderate or mild and last for about two days following vaccination. Previous research has indicated a few cases of isolated pituitary abnormalities, such as hypophysitis.
Hypophysitis is a rare and chronic inflammatory condition of the pituitary gland that causes anterior and/or posterior pituitary hormonal deficiencies and structural changes in the hypothalamic-pituitary axis. This condition is highly heterogenous and can be caused by several medical treatments.
A recent study reported cases of pituitary lesions associated with COVID-19 vaccination. However, no data is available on the occurrence of hypophysitis yet. Moreover, this was the fourth reported case of hypophysitis post-SARS-CoV-2 vaccination and the second one associated with central diabetes insipidus.
A new study to be published in the Therapies journal aimed to analyze a rare case of hypophysitis caused by pituitary stalk thickening three days following the administration of the SARS-CoV-2 vaccine.
About the study
The study involved a 54-year-old female previously diagnosed with high blood pressure and treated with a calcium channel blocker. She reported no family or personal history of COVID-19, endocrine disease, autoimmune diseases, or upper respiratory tract infections. Three days after receiving the first SARS-CoV-2 vaccine (Oxford-AstraZeneca ChAdOx1 nCoV-19), she reported the onset of nycturia and polyuria of almost 10 liters per day.
Thereafter, she underwent several tests that involved blood pressure, body mass index (BMI), osmolarity, vasopressin challenge, total blood count, antinuclear antibody, liver function, endocrine function, chest radiography, cortisol stimulation, and water deprivation test. Finally, the diagnosis of central diabetes insipidus (DI) was carried out, followed by magnetic resonance imaging (MRI) of the pituitary stalk.
Study findings
The results indicated that her blood pressure was 130/70 mm Hg, pulse rate was 90 beats per minute, BMI was 36 kg/m², levels of plasma osmolarity and serum sodium were high (305.8 mosmol/kg and 151 mmol/L, respectively), as well as levels of urine osmolarity were low (138 mosmol/kg). The water deprivation test had to be stopped at the third hour due to excessive thirst intolerance. Moreover, the urine osmolarity was observed not to increase above 200 mosmol/ kg irrespective of 1 kg weight loss in 3 hours.
DI diagnosis was confirmed through urine output and vasopressin challenge test. Furthermore, the MRI of the pituitary stalk showed 5.05 mm of thickening in the transverse dimension, which was suggestive of infundibuloneuro hypophysitis. The serum levels of angiotensin-converting enzyme, β2 microglobulin, and IgG4 were reported to be normal. The chest radiography, total blood count, liver function, endocrine function, and antinuclear antibody test results were also reported to be normal. Furthermore, treatment with oral desmopressin at 60 mg /day showed a decrease in thirst, and with 120 mg/day complete remission of DI symptoms was observed.
Conclusion
Therefore, the current study suggests that the onset of hypophysitis is brought about by adjuvants of the SARS-CoV-2 vaccine since the signs for all other potential etiologies were absent. Further research must be done on the autoimmune and endocrine effects of the mRNA COVID-19 vaccine to prevent such side effects.