In healthcare settings, clinicians often need to image a patient's internal organs. To do this, ultrasound imaging is frequently used. Can you tell us more about how ultrasound imaging works?
Ultrasound imaging is a safe and noninvasive window into the body's workings, providing clinicians with live images of a patient's internal organs. To capture these images, trained technicians manipulate ultrasound wands and probes to direct sound waves into the body. These waves reflect back out to produce high-resolution images of a patient's heart, lungs, and other deep organs.

Image Credit: HOMONSTOCK/Shutterstock.com
Despite ultrasound imaging being commonplace within healthcare settings, it has many disadvantages. What are some of these disadvantages, and how does your new technology help to overcome them?
Conventionally, to image with ultrasound, a technician first applies a liquid gel to a patient's skin, transmitting ultrasound waves. A probe, or transducer, is then pressed against the gel, sending sound waves into the body that echo off internal structures and back to the probe, where the echoed signals are translated into visual images.
For patients who require long periods of imaging, some hospitals offer probes affixed to robotic arms that can hold a transducer in place without tiring, but the liquid ultrasound gel flows away and dries out over time, interrupting long-term imaging.
To solve this problem, we designed an ultrasound sticker that produces higher-resolution images over a longer duration by pairing a stretchy adhesive layer with a rigid array of transducers. This combination enables the device to conform to the skin while maintaining the relative location of transducers to generate clearer and more precise images.
In your latest research, you have designed a new ultrasound sticker. How did you design this sticker, and how does it work?
We designed a new ultrasound sticker that produces high-resolution images over a longer duration by pairing a stretchy adhesive layer with a rigid array of transducers. This combination enables the device to conform to the skin while maintaining the relative location of transducers to generate clearer and more precise images.
The device's adhesive layer is made from two thin layers of elastomer that encapsulate a middle layer of solid hydrogel, a mostly water-based material that easily transmits sound waves. The MIT team's hydrogel is elastic and stretchy, unlike traditional ultrasound gels. The elastomer prevents dehydration of hydrogel. When hydrogel is highly hydrated, acoustic waves can penetrate effectively and give high-resolution imaging of internal organs.
The bottom elastomer layer is designed to stick to the skin, while the top layer adheres to a rigid array of transducers that the team also designed and fabricated. The entire ultrasound sticker measures about 2 square centimeters across and 3 millimeters thick — about the area of a postage stamp.
To test our design, we put the ultrasound sticker through a battery of tests with healthy volunteers, who wore the stickers on various parts of their bodies, including the neck, chest, abdomen, and arms. The stickers stayed attached to their skin and produced clear images of underlying structures for up to 48 hours.
Ultrasound Sticker
Your ultrasound sticker can also provide continuous imaging of internal organs for 48 hours, as well as capture images when a patient performs various activities. How is this possible, and what advantages does it have for clinicians by observing organs over a period of time compared to a single snapshot moment?
Our BAUS system enables this, and an adhesive ultrasound sticker can be applied on the human skin, stay stable, and image internal organs continuously. An imaging device that maintains a continuous watch over specific body parts could be used to monitor and diagnose various diseases. Doctors could keep a close eye on the growth of a tumor over time.
Someone at high risk of hypertension might wear an ultrasound patch to measure their high blood pressure, alerting them when the pressure spikes or tracking whether a medication is helping. A COVID patient could stay home, knowing that an imaging device would alert them if their illness caused a lung infection severe enough to require hospitalization.
Are you hopeful that with continued research into these ultrasound stickers, they could be offered in pharmacies so patients do not need to visit a healthcare setting? What advantages would this have for both patients and clinicians?
Yes, we hope BAUS could be one of the future health monitors that can be bought at a pharmacy. Therefore, we are designing mass production capabilities to further cut down the cost, given the current sticker costs around 200 USD each. The big selling point/advantage of this new device is that it opens new types of medical diagnoses that can't be done in a static setting.
To assess heart health, for instance, it's helpful to measure the organ's activity while exercising—but it's hard to hold an ultrasound wand against a running subject's goo-covered chest. With a wearable ultrasound patch, where you wouldn't have to hold the transducer on the person, they could show that you're able to get high-quality images of the heart even during motion. The technology can reduce the burdens of both clinicians and patients.
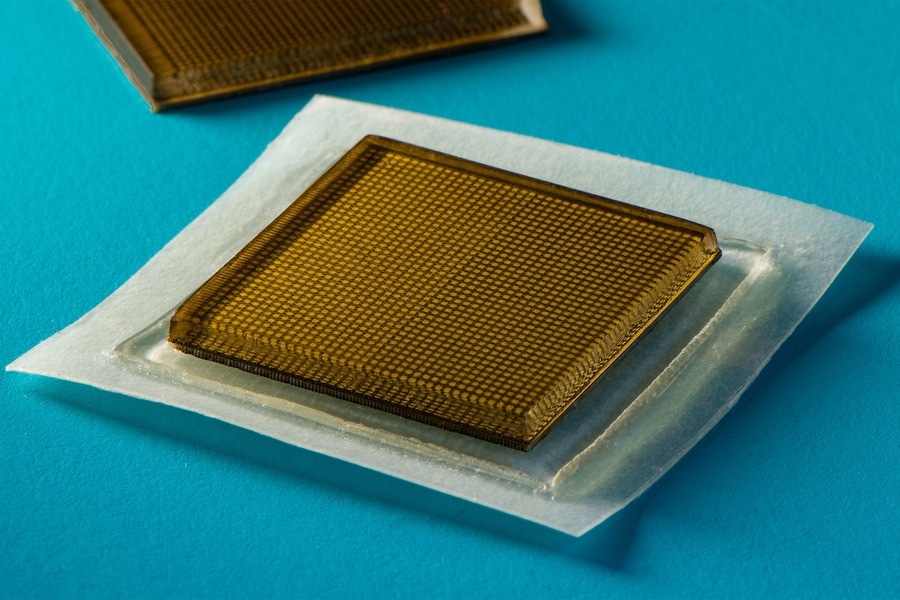
Image Credit: Felice Frankel/Shutterstock.com
Medical wearables have seen a huge increase in attention in recent years, thanks partly to artificial intelligence and machine learning. How could both of these disciplines be applied to your ultrasound sticker to further its development?
A big direction we are working on is the application of artificial intelligence into the BAUS system. An image is only worth something if you can actually diagnose it. So even if we can get all these images, we still need help getting useful medical diagnoses out of them.
We are building algorithms that could track organ physiology, quantitively analyze it, and arrive at a diagnosis decision. This will save the burden on the clinician.
Do you believe your technology could potentially help to improve clinical diagnoses worldwide? What could this mean for global health?
The most important application we envisioned could be in detecting and diagnosing heart attacks. Heart health is on the radar of other wearable device developers. For instance, smartwatches such as the Apple Watch are capable of tracking the electrical signals that indicate heart activity with a so-called electrocardiogram (ECG or EKG). This can be used to diagnose heart attacks—at least in some cases.
Studies show that EKG can only diagnose around 20 percent of heart attacks. The majority of heart attacks actually require imaging modalities, such as ultrasound imaging, to diagnose. Continuous imaging of a patient's heart could capture their symptoms and provide an early diagnosis. We envision ultrasound stickers could be packaged and purchased by patients and consumers and used not only to monitor various internal organs but also the progression of tumors, as well as the development of fetuses in the womb.
Your research was funded in part by MIT but also by various organizations, including the NIH, the U.S. Army Research Office, and the National Science Foundation. How important is funding in discovering new scientific technologies?
Funding is essential to enable the understanding of fundamental science and the development of technology that will address grand societal challenges. We greatly appreciate various funding agencies that trust us and support our work.
What are the next steps for you and your research?
We are working on a fully integrated BAUS system that anyone could use, and we are also working with clinicians to obtain clinical data and push the device to clinical trials.
Where can readers find more information?
Our group's website: http://zhao.mit.edu/
About Professor Xuanhe Zhao
Xuanhe Zhao is a professor of mechanical engineering and civil and environmental engineering (by courtesy) at MIT. The mission of Zhao Lab at MIT is to advance science and technology on the interfaces between humans and machines for addressing grand societal challenges in health and sustainability with integrated expertise in mechanics, materials and biotechnology. A major focus of Zhao Lab's current research is the study and development of soft materials and systems. 
About Chonghe Wang
Chonghe Wang is currently a graduate student researcher working with Prof. Xuanhe Zhao at Mechanical Engineering department of Massachusettes Institutes of Techonology. Chonghe has more than 10 years of research experience in ultrasound technology.
From 2016, he pioneered the direction of engineering wearable ultrasound technology that could monitor deep tissue vital signs in the human body. His leading research work was published in Science (2022), Nature Biomedical engineering (2021), Nature Biomedical engineering (2018) and was exclusively highlighted by hundreds of famous media including: National Geographic Magazine, Forbes, MIT Technology Review, National Institute of Health (NIH), and many others. This technology has huge potential of shifting the paradigm of transforming bulky clinical ultrasound machine to wearable smart devices for next generation digital healthcare.
His works have been accepted and published by series of notable journals includes Nature, Science, Nature Biomedical Engineering, Nature Nanotechnology, Nature Electronics, Science Advances, Proceeding of National of Academy of Science, Advanced Materials, and many others. He was recognized as the '2019 Baxter Young Investigator' for his contribution in developing the world first wearable central blood pressure monitor that could potentially save lives of ICU patient.
About Dr. Xiaoyu Chen
Xiaoyu Chen is a postdoctoral fellow in the Department of Mechanical Engineering at Massachusetts Institute of Technology. He received his B.S. degree in the College of Chemistry at Jilin University in 2013. He earned his Ph.D. degree in the Department of Biomedical Engineering at the Chinese University of Hong Kong in 2019. His research focuses on the design and preparation of polymeric biomaterials for biomedical applications. He is a recipient of the CUHK Outstanding Student Award and the Society for Biomaterials STAR Award.