Studies have reported elevated LDG counts in severe SARS-CoV-2 infections; however, the long-term impact of coronavirus disease 2019 (COVID-19) on LDG expression and phenotypic alterations has not been well-characterized. Further research is required to assess the functional contributions of LDGs to pulmonary post-acute sequelae of COVID-19 (PPASC) development.
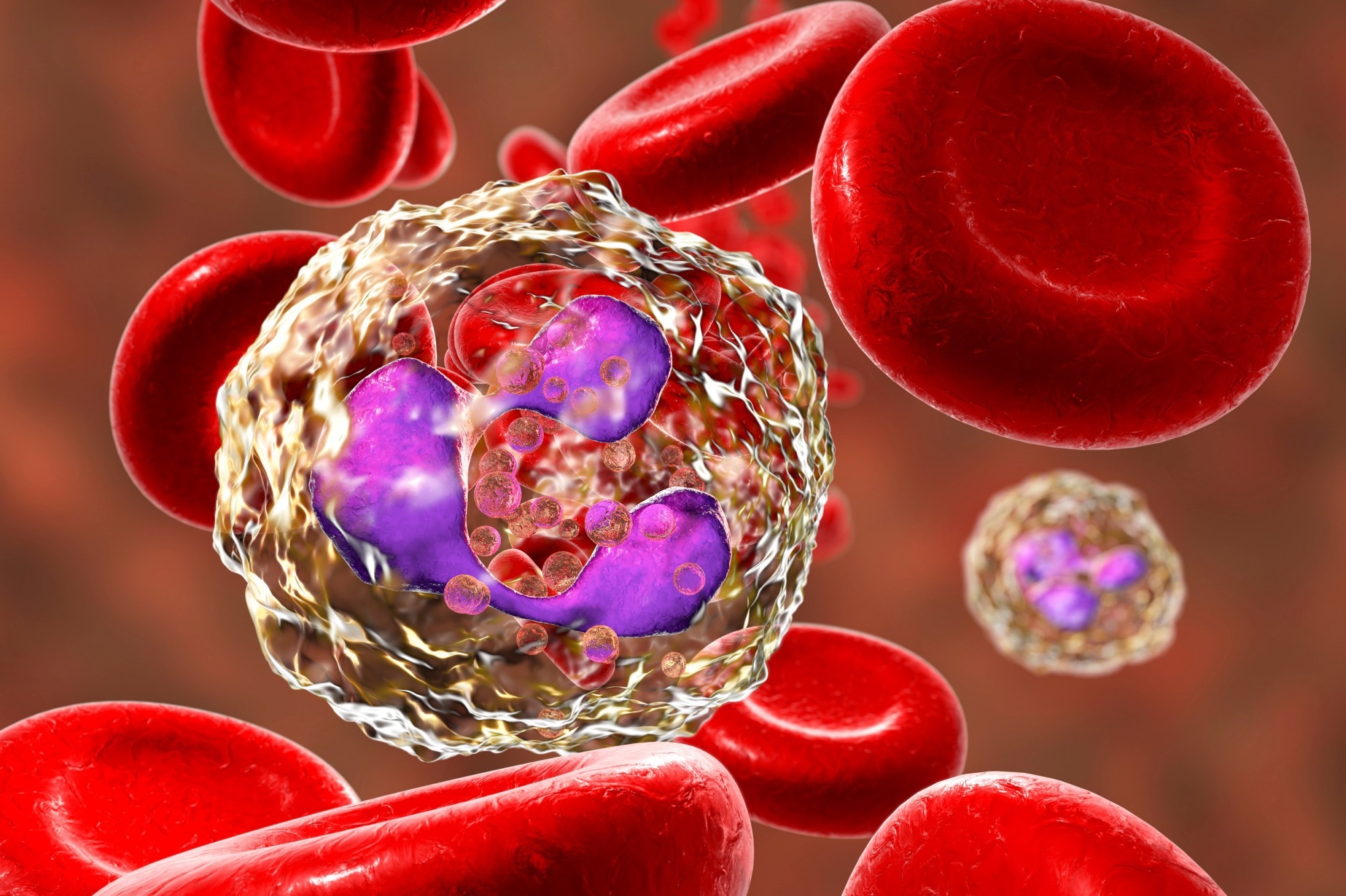 Study: Phenotypic alteration of low-density granulocytes in people with pulmonary post-acute sequalae of SARS-CoV-2 infection. Image Credit: Kateryna Kon / Shutterstock
Study: Phenotypic alteration of low-density granulocytes in people with pulmonary post-acute sequalae of SARS-CoV-2 infection. Image Credit: Kateryna Kon / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
About the study
In the present cross-sectional study, researchers explored LDG levels and their association with PPASC symptoms.
The study comprised 12 SARS-CoV-2 infection convalescent individuals with pulmonary symptoms and 10 recovered individuals without residual COVID-19 symptoms (NRS). For comparison, 12 human immunodeficiency virus (HIV)-negative individuals from a previously conducted study were included as SARS-CoV-2-naïve controls (NP).
The study participants filled out questionnaires concerning demographics, medical history, and acute or long-term SARS-CoV-2 infection symptoms. PPASC patients were identified based on pulmonary function tests (PFTs), especially lowered DLCO (diffusing capacity for carbon monoxide) values after 30 days of acute COVID-19.
Whole blood samples were obtained from the participants, and their peripheral blood mononuclear cells (PMBCs) were isolated. Subsequently, plasma cell-free deoxyribonucleic acid (cfDNA) and CitH3 were quantified to investigate if NP extracellular trap (NET) concentration was elevated in SARS-CoV-2 infection convalescents due to elevated LDG numbers with increased NET-releasing ability.
Further, flow cytometry (FC) analysis and enzyme-linked immunosorbent assays (ELISA) were performed to compare LDG levels and their phenotypes based on markers of activation, maturation, and NET formation. In addition, LDG activation was assessed based on the myeloperoxidase (MPO) and cluster of differentiation 11b (CD11b) expression and LDG granularity.
Furthermore, the team investigated whether NET formation was higher among PPASC patients. They also investigated whether platelet-NP aggregation (PNA) is facilitated by activated platelets in SARS-CoV-2 infections by examining P-selectin (CD62P) expression on platelets bound to NET-forming LDGs.
Results
The median values for participant age of in the NRS, PPASC, and NP groups were 55, 55, and 57 years, respectively, and most (84%) of them were men. LDG counts were significantly higher among PPASC patients than NP individuals. PPASC and NRS individuals showed elevated counts of CD10+ and CD16HI LDG subsets compared to controls.
PPASC patient LDGs showed enhanced NET-forming capability and platelet aggregation than NRS and NP group individuals. LDGs showed CD11b+/CD14-/CD15+/CD16+/CD45+ expression. PPASC patients showed a rising trend in LDG proportion (one percent) and significantly higher LDG counts than controls (1243 vs. 372).
Of interest, LDG numbers were higher, although not significantly, among NRS individuals compared to controls, although with similar frequency as controls, indicative of a preferential LDG expansion among NRS individuals. CD10+ LDG frequency was significantly higher among PPASC and NRS individuals than among controls.
Likewise, CD10+ LDG numbers were significantly higher among PPASC (684) and NRS (337) group individuals than controls (105). PPASC and NRS LDGs showed greater CD10 median fluorescence intensity (MFI) scores than controls. In addition, C16 and CD15 MFI scores per granulocyte were significantly greater among PPASC patients than controls, although an increasing trend of elevated expression was observed in the NRS group.
The findings indicated that LDGs showed an elevated frequency of mature LDGs, and their counts persisted at high levels for several months post-COVID-19, even among recovered NRS COVID-19 patients lacking residual COVID-19 symptoms. The PPASC and NRS group individuals showed more mature LDG NPs than controls, and the CD16hi and CD16lo LDG subsets showed higher expression among PPASC patients.
CD16hi LDGs from PPASC patients showed mature NP phenotypes with CD10 expression. COVID-19 convalescent individuals showed an elevated expression of mature phenotype LDGs with greater MFI scores for MPO, indicative of greater granularity of COVID-19 convalescent individual NPs. LDGs that formed NETs showed double positivity for MP0 and CitH3 (citrullinated histone H3). NET-forming LDG frequency was lower among PPASC patients.
However, the corresponding LDG counts were significantly elevated among PPASC and NRS than NP individuals. NP activation, LDG-bound platelets, CitH3, and cfDNA expression were greater among PPASC patients than among controls. P-selectin MFI scores did not differ significantly among the groups, indicating that PNA was independent of platelet P-selectin expression.
Overall, the study findings showed that a persistent increase in NP activation markers and NET formation on LDGs and a heightened PNA formation proclivity among PPASC individuals might be associated with long-term pulmonary COVID-19 sequelae development.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Phenotypic alteration of low-density granulocytes in people with pulmonary post-acute sequelae of SARS-CoV-2 infection. Logan S. Dean et al. bioRxiv preprint 2022, DOI: https://doi.org/10.1101/2022.10.22.513351, https://www.biorxiv.org/content/10.1101/2022.10.22.513351v1
- Peer reviewed and published scientific report.
Dean, Logan S., Gehan Devendra, Boonyanudh Jiyarom, Natalie Subia, Michelle D. Tallquist, Vivek R. Nerurkar, Sandra P. Chang, Dominic C. Chow, Cecilia M. Shikuma, and Juwon Park. 2022. “Phenotypic Alteration of Low-Density Granulocytes in People with Pulmonary Post-Acute Sequalae of SARS-CoV-2 Infection.” Frontiers in Immunology 13 (December). https://doi.org/10.3389/fimmu.2022.1076724. https://www.frontiersin.org/articles/10.3389/fimmu.2022.1076724.