Background
An emerging concern associated with the coronavirus disease 2019 (COVID-19) pandemic is long COVID or clinical sequelae consisting of chronic fatigue, memory loss, muscle weakness, reduced pulmonary capacity during exertion, persistent fever, myalgia, epileptic seizures, stroke, and other cardiovascular complications. Patients who have recovered from severe COVID-19 experience these debilitating symptoms for months after recovery.
Furthermore, studies that examined vaccinated individuals who experienced breakthrough severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections found a high incidence of long COVID symptoms such as deteriorated musculoskeletal, neurological, and mental health among these individuals after recovery. This indicates that vaccination provides only limited protection against long COVID.
Melatonin is a cryoprotective hormone and chemical that exhibits anti-inflammatory, antioxidant, and immunoregulatory activity and has been seen to impair viral infections, play a role in circadian rhythm maintenance, and be effective against diabetes mellitus and cardiovascular diseases. It is also involved in the activation of glutathione-synthesizing enzymes. Melatonin could potentially be a therapeutic agent in treating long COVID symptoms.
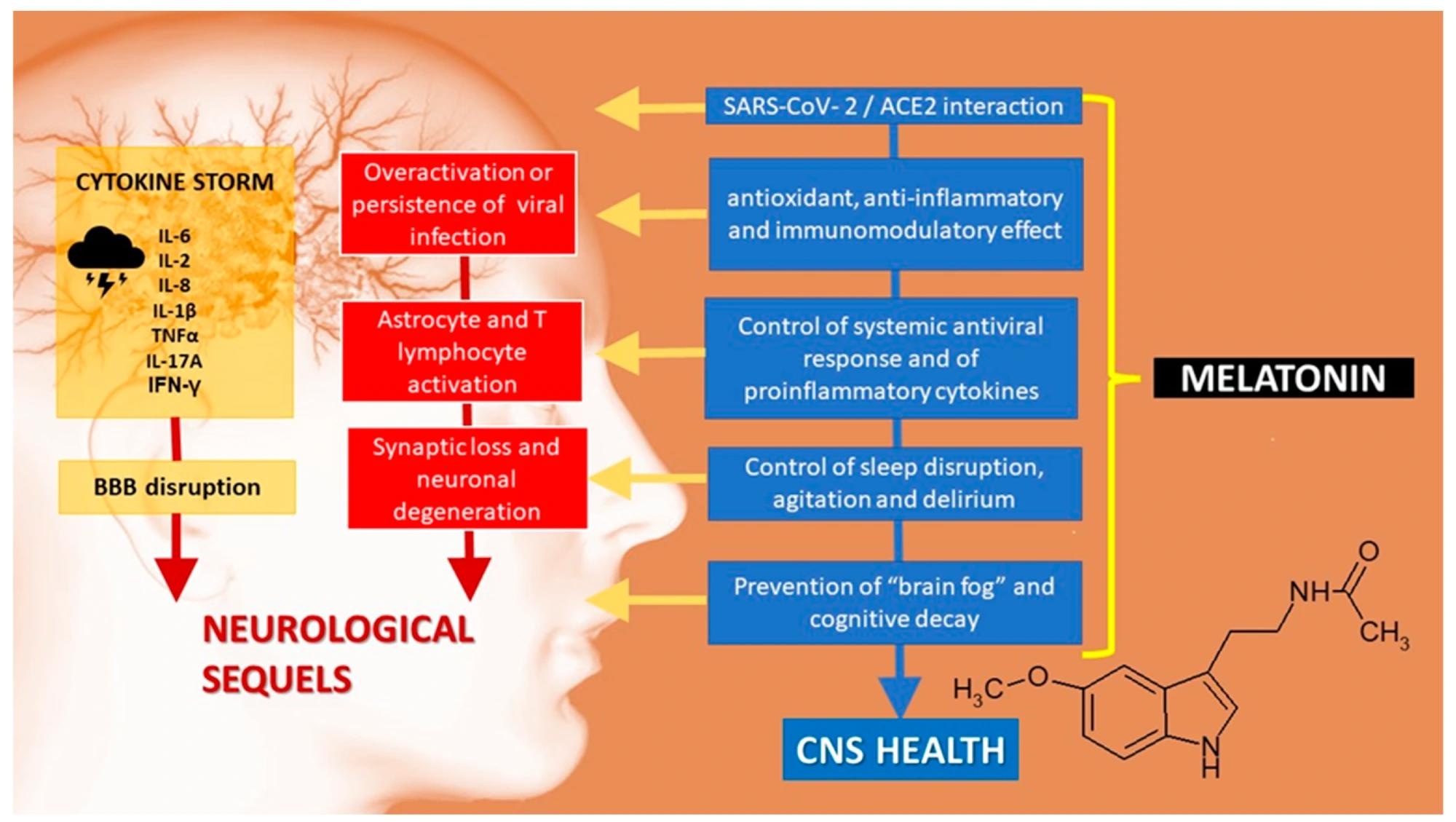
Central nervous system sequelae of SARS-CoV-2 infection. ACE2: angiotensin-converting enzyme 2. BBB: blood–brain barrier.
Long COVID symptoms
Brain fog is a general term used to defineimpaired cognitive function, such as difficulty concentrating, loss of working and short-term memory, and difficulty with verbal and non-verbal methods of learning and mathematical problem-solving. While brain fog can be a consequence of various factors such as sleep deprivation, malnutrition, pregnancy or menopause-related hormonal changes, or even chemotherapy, it was the most reported symptom among COVID-19-recovering patients with no history of other diseases or hypoxia.
An intelligence test in the United Kingdom detected cognitive impairments in a significant number of individuals with COVID-19. Symptoms included memory loss, disorientation, and reduced mental energy.
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is characterized by excessive and persistent fatigue, inability to perform physical exercise, and autonomic dysregulation. ME/CFS is also associated with disruption of circadian rhythms and the gut/mucosal barrier, mitochondrial dysfunction, and a pro-inflammatory state. Studies indicated that 45% of COVID-19 patients who were hospitalized and required intensive care unit admission exhibited ME/CFS symptoms up to six months after recovery.
Melatonin as a potential long COVID treatment
Melatonin is a hormone naturally produced in all aerobically respiring life forms, and it performs antioxidant, anti-inflammatory, immunostimulant, and neuroprotective functions in the body. It reduces the pro-inflammatory response of macrophages, activates nuclear erythroid 2-related factor 2, and suppresses the activation of nuclear factor (NF)-κB. Melatonin is also known to balance inflammatory responses by decreasing the levels of pro-inflammatory cytokines such as interleukins (IL) 1β, 6, and 8, and tumor necrosis factor (TNF)-α, and increasing anti-inflammatory cytokine IL-10.
Warburg’s effect during viral infections causes a shift from mitochondrial oxidative phosphorylation to glycolysis which occurs in the cytoplasm. This is accompanied by inflammation-promoting mechanisms such as an increase in NF-κB and hypoxia-inducible factor-1α. Consequently, the anti-inflammatory M2 macrophages are converted to pro-inflammatory M1 macrophages, causing a cytokine storm known to cause endothelial tissue and organ damage in severe COVID-19 patients.
The anti-inflammatory effects of melatonin in preventing pro-inflammatory profiles or macrophages and suppressing NF-κB activation can help reverse Warburg’s effect in long COVID patients.
Melatonin also regulates the amyloid β (Aβ) metabolism associated with Alzheimer’s disease. Studies with transgenic Alzheimer’s disease models have shown that melatonin can control neuroinflammation by interacting with Aβ40 and Aβ42 and increasing protein degradation. Furthermore, the ability of melatonin to regulate circadian rhythms and sleep patterns has been shown to improve cognitive function and sleep in patients in the early stages of cognitive decline.
Melatonin is also known to exhibit therapeutic activity against the various symptoms of ME/CFS, such as oxidative stress, pro-inflammatory state, mitochondrial and bioenergetic dysregulation, and disruption of the gut/mucosal barrier.
Conclusions
Overall, the review reported the significant potential for the use of melatonin in long-COVID and COVID-19 therapy. Studies have shown melatonin is more effective in reducing COVID-19 inflammatory markers than commonly used SARS-CoV-2 antivirals.
The authors believe that although melatonin exhibits anti-inflammatory and immunostimulant properties that many studies have reported being effective against COVID-19, it has not been promoted as a therapeutic option, possibly due to its easy availability and non-patentability, which makes it an unattractive target for pharmaceutical industries. They recommend clinical trials to explore the use of melatonin as a treatment for long COVID symptoms.