The first suspected MPX case in the US was identified in May 2022, with the Centers for Disease Control and Prevention (CDC) initiating an emergency response. More than 29,900 cases of MPX have been reported to the CDC to date, with daily case counts peaking in August. In the present study, researchers described the epidemiologic features of the ongoing MPX outbreak and the public health response in the US.
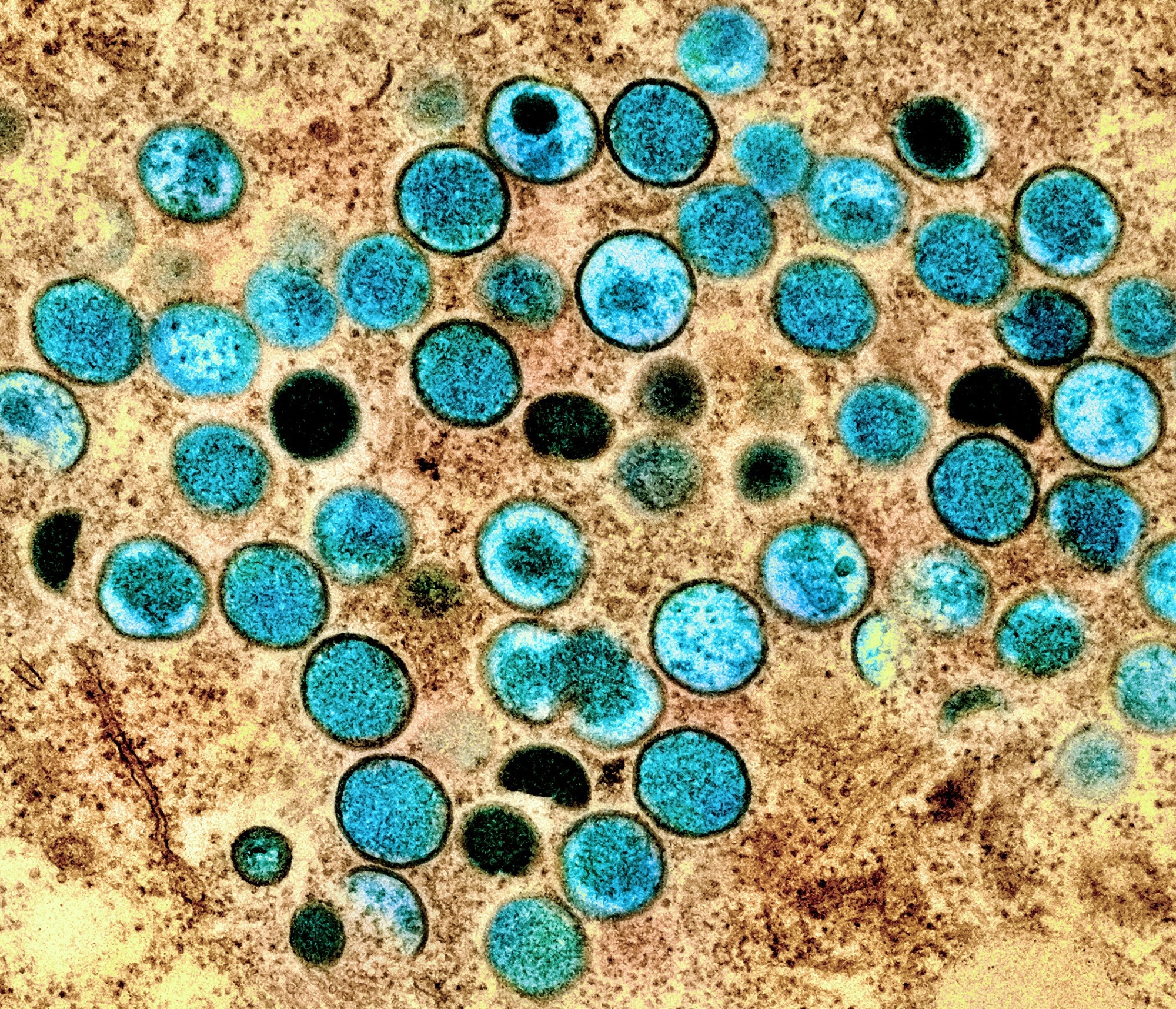 Study: Epidemiologic Features of the Monkeypox Outbreak and the Public Health Response — United States, May 17–October 6, 2022. Image Credit: NIAID
Study: Epidemiologic Features of the Monkeypox Outbreak and the Public Health Response — United States, May 17–October 6, 2022. Image Credit: NIAID
Epidemiology of MPX cases
The Council of State and Territorial Epidemiologists approved designating MPX as a nationally notifiable disease on June 23, 2022. Around 26,384 MPX cases were reported to the US CDC between May 17 and October 6, 2022. The authors described and compared MPX case characteristics pre- and post-July 18, when testing capacity and access substantially increased.
The median age of patients was 34. The proportion of MPX cases among those aged 18 to 29 increased from 20% to 27% after July 18, whereas that of 30-39-year-old MPX cases dropped to 41%. Information on ethnicity and race was available for 21,211 patients; 32% of cases were Black, 31% were Hispanics, and 30% were White.
The proportion of Black individuals with MPX increased from 21% to 35% after July 18, while that of Hispanic and White people with MPX decreased to 31% (from 33%) and 28% (from 39%), respectively. Gender information was available for 25,569 MPX cases, with 95% of cases identifying as cisgender males. More than 10,400 cisgender males reported having male-to-male sexual contact (MMSC) in the past 21 days of symptom onset.
The proportion of cisgender males reporting recent MMSC declined over time. 13,871 MPX cases had a rash most frequently observed on the face, genitals, and arms. Data on human immunodeficiency virus (HIV) infection was available for 5017 cases; 57% were HIV-positive among these. More than 1,800 MPX cases were hospitalized, and six deaths were documented. MPX or smallpox vaccination status was available for 9,197 patients, with 2882 cases having been vaccinated.
Public Health Response
The US CDC launched an emergency response to MPX within a week of identifying the first suspected case. Besides the enhanced surveillance, the emergency response was focused on expanding laboratory testing, medical countermeasures for post-exposure prophylaxis and treatment, and dissemination of information to the public and healthcare providers.
A US Food and Drug Administration (FDA)-approved polymerase chain reaction (PCR) test detecting non-variola Orthopoxviruses was available before the MPX outbreak as a consequence of smallpox preparedness efforts. The CDC provided technical support to increase testing capacity. In addition, the JYNNEOS vaccine, stockpiled for use in immunocompromised individuals in case of a smallpox outbreak, was available to tackle the MPX outbreak.
The JYNNEOS vaccine, to be administered intradermally, was authorized for emergency use on August 9, 2022. More than 931,100 MPX vaccine doses have been administered until October 10, 2022. While no FDA-approved therapeutic products for MPX exist, tecovirimat, approved for smallpox in 2018, has been recommended for use in patients at risk of or with severe MPX. A randomized controlled clinical trial is underway to assess the efficacy of tecovirimat for MPX treatment.
The CDC leverages numerous mechanisms to disseminate information about MPX to healthcare providers and the public. The CDC issued the first Health Alert Network Health Advisory on May 20, 2022, with four subsequent releases. Moreover, the CDC hosts clinician outreach and communication activity calls, wherein subject matter experts present the latest information and considerations. Around 10,000 healthcare professionals attended the first such call.
Concluding remarks
Prior knowledge of sexually-transmitted infections and MPX, diagnostic/laboratory support, medical countermeasures, and outreach have been instrumental in CDC’s response to MPX. CDC continues to analyze new evidence and interventions for MPX prevention and control. Prevention efforts must emphasize vaccination for at-risk populations. Efforts are required to reduce the stigma about MPX and ensure equitable access to testing, treatment, and vaccination.