Research suggests that some patients with coronavirus disease 2019 (COVID-19) develop a post-COVID-19 syndrome (long COVID), a state of chronic fatigue characterized by post-exertional neuro-immune exhaustion. Fatigue, breathlessness, brain fog, chest pain, cough, gastrointestinal symptoms, headache, and musculoskeletal pain are the commonly experienced symptoms.
Initially, much evidence about long COVID emerged from patient-led research, self-reports in social media, and medical blogs. In the United Kingdom, the Office for National Statistics (ONS) estimated that 13.7% of infected individuals experience long COVID. Risk factors associated with symptoms lingering beyond the acute phase include female sex, older age, asthma, previous heart/lung disease, and COVID-19 severity.
The ZOE COVID-19 symptom tracker app is a promising avenue to examine long COVID symptoms. More than four million people have downloaded it and are encouraged to track daily symptoms. This dataset has been instrumental in multiple COVID-19-related studies in identifying predictors of hospitalization, symptom clusters, vaccine efficacy, and side effects, among others.
 Study: Risk factors and symptom clusters for Long Covid: analysis of United Kingdom symptom tracker app data. Image Credit: p.ill.i / Shutterstock
Study: Risk factors and symptom clusters for Long Covid: analysis of United Kingdom symptom tracker app data. Image Credit: p.ill.i / Shutterstock

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
About the study
In the present study, researchers at Brighton and Sussex Medical School and the University of Sussex evaluated risk factors associated with long COVID and determined if data from the ZOE symptom tracker app provided evidence of different long COVID sub-types. Users of the ZOE COVID-19 symptom tracker app receive daily prompts asking them to log symptoms. Data entered by users during app registration and daily entries were used for analyses.
Participants were required to have logged on for a minimum of 120 days overall, tested SARS-CoV-2-positive between July 1 and December 11, 2020, with a body mass index (BMI) between 15 and 55, and logged within seven days of the positive test. In addition, the sampled population was tested for selection bias against a reference sample that included anyone who logged on at least 120 days and tested positive from July 1, 2020, to January 1, 2021.
The authors defined long COVID as experiencing a statistically more significant proportion of negative health status during weeks 12 to 15 post-COVID-19 relative to weeks 2 to 12 pre-COVID-19. Two-tailed Proportions Z test was used for categorical data, and the two-tailed Mann-Whitney U test was used for continuous data for univariate analysis of risk factors. In addition, logistic regression with LASSO penalization was used to evaluate multiple predictors.
Multivariable models were run with two blocks – the first block included demographic variables and medical history (without symptom data), and the second block contained symptom scores in weeks 0 to 8 after the positive test. The authors relied on K-modes clustering, factor analysis, and hierarchical agglomerative clustering for cross-comparison between methods and to assess how robust any symptom cluster was likely to be for their second objective to explore evidence of long COVID subtypes.
Findings
The researchers identified 4,040 app users after applying eligibility filters. Most app users were female (59.5%) and white (97.5%). Participants mostly lived in areas of higher income levels. 13.6% of the sample satisfied the criteria set for long COVID; 15.1% of the long COVID cohort had no symptoms when testing SARS-CoV-2-positive. Participants in the long COVID cohort initially recovered from symptoms within three to four weeks of the positive test.
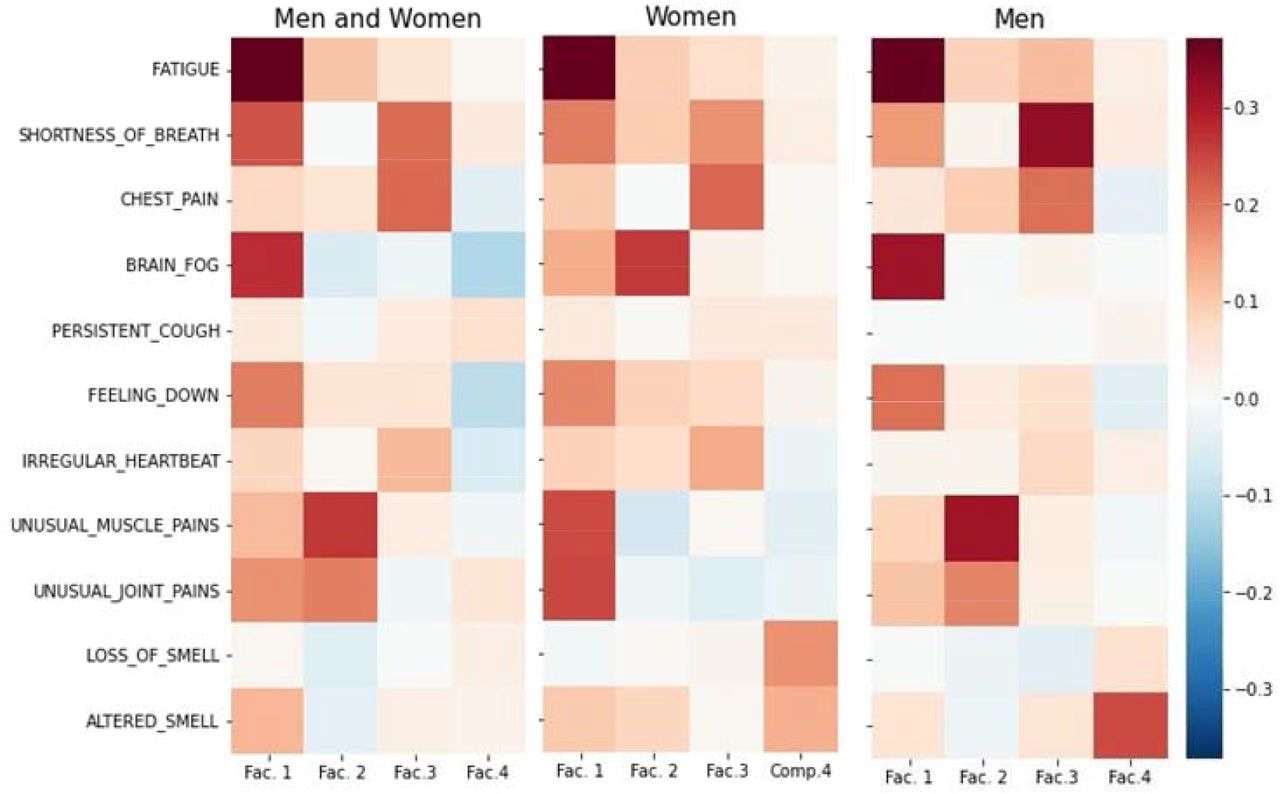 Factor Analysis heatmap showing loading of symptoms onto factors
Factor Analysis heatmap showing loading of symptoms onto factors
Univariate analyses revealed a significant association between long COVID and female sex, hay fever, prior lung disease, asthma, intake of vitamin D or other vitamins, and previous limited activity. There was a weak association of long COVID with age and BMI. Symptoms during weeks 0 to 8 post-infection strongly predicted long COVID. Olfactory issues and fatigue were the strong predictors of long COVID from weeks 4-6 onwards.
The authors observed a positive association between long COVID and pre-existing medical conditions for all subjects up to 70 years but a negative association for those above 70 years. The multivariable model run with demographics and medical history retained gender, limited activity, vitamin D intake but not others, and baseline health status. The retained variables in the model with symptom data were the same as the model without symptom data, except for the addition of max symptom score in the first two weeks post-infection.
Conclusions
The authors identified the female sex, pre-existing medical conditions, limited physical activity before COVID-19, and more symptoms during COVID-19 as factors associated with an increased risk of progressing to long COVID after 12 weeks of COVID-19. The accuracy of prediction of long COVID was 69% at the onset of COVID-19, and 77% after eight weeks of symptoms, with the highest error rate in those with asymptomatic infection.
Overall, the study found that sex, baseline health status, symptoms, and previous limited activity could predict long COVID in those with symptomatic COVID-19 with reasonable accuracy. Notably, symptom severity during the first eight weeks of illness was the strongest predictor of long COVID. There was no evidence to suggest more than one type of long COVID among patients.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.