In a recent study published in the JAMA Network Open journal, researchers evaluated the relationship between congenital cytomegalovirus (cCMV) infection and acute lymphoblastic leukemia (ALL).
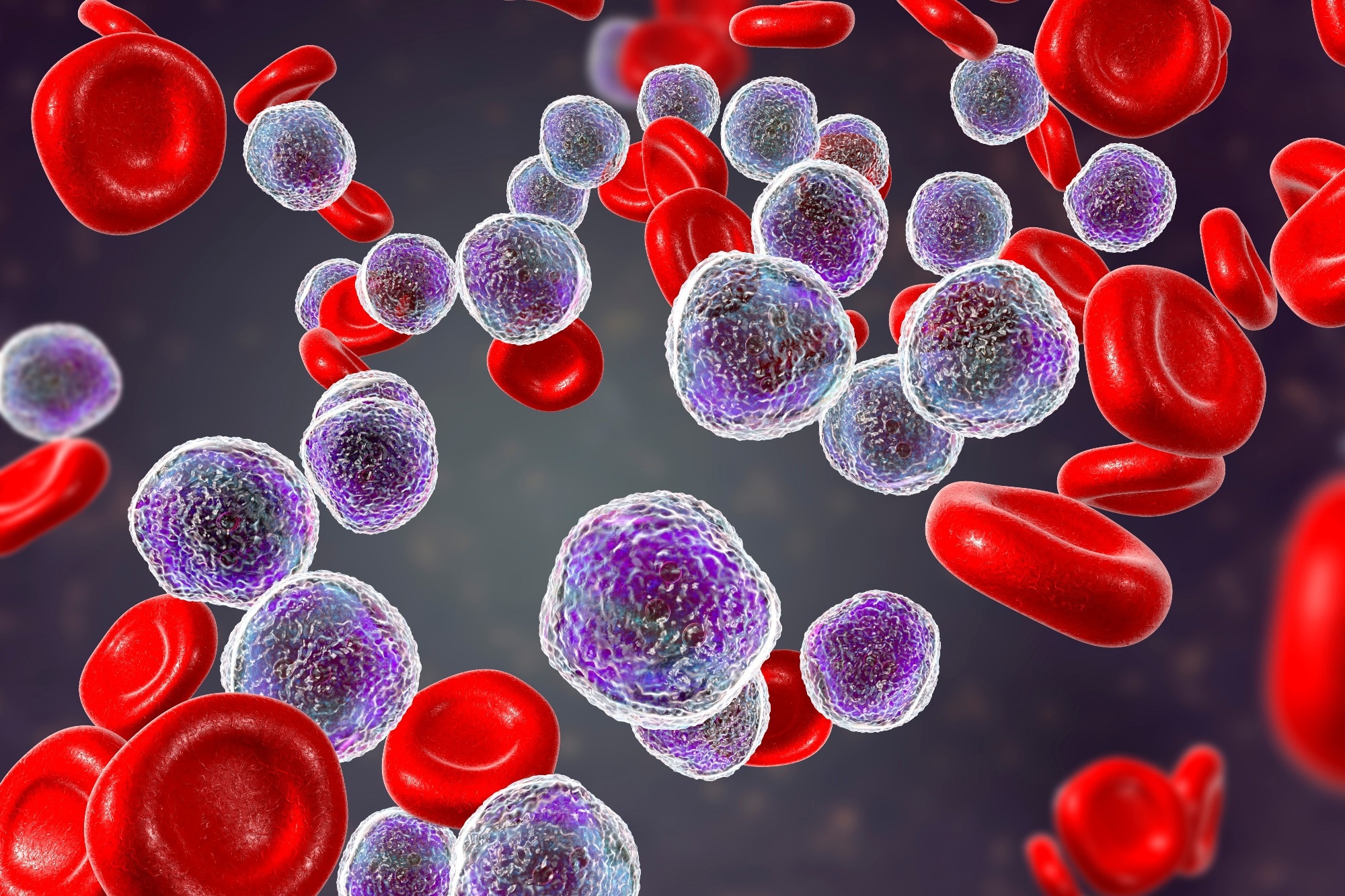 Study: Evaluation of the Association Between Congenital Cytomegalovirus Infection and Pediatric Acute Lymphoblastic Leukemia. Image Credit: Kateryna Kon/Shutterstock
Study: Evaluation of the Association Between Congenital Cytomegalovirus Infection and Pediatric Acute Lymphoblastic Leukemia. Image Credit: Kateryna Kon/Shutterstock
ALL is the most prevalent form of cancer among children, accounting for about 20% of malignant neoplasms observed in individuals under the age of 20. Genetic predispositions with a high penetrance, like Down syndrome, account for fewer than 5% of ALL instances. Environmental risk factors, such as ionizing radiation exposure, have also been postulated; however, the data is inconclusive. Almost ALL instances' causes remain mostly unclear. CMV has arisen as a possible risk factor for ALL in recent years. CMV belongs to the family of herpesviruses (HHV 5) and can cause transplacental infection at the time of pregnancy. Studies indicate that prenatal CMV infection significantly raises the chances of suffering from pediatric ALL. As cCMV screening among newborns is under development, it is crucial to determine by replication if CMV infection at birth can lead to ALL.
About the study
In the present study, researchers determined the predominance of cCMV infection among ALL patients and matched controls.
Infection with cCMV was evaluated in a population-based case-control research conducted by the Michigan BioTrust for Health (MBH). Cases included children aged between zero and 14 years, born on or after 1 October 1987 in Michigan and diagnosed with ALL. Case-specific cytogenetic and molecular information was extracted. MBH chose four-to-one matched controls based on birth year, gender, and the mother's reported ethnicity and race.
For efficient adjustment of confounding, the sex, race, and ethnicity of the mother were matched, whereas the birth year was matched to have equal windows of exposure. The birth registry was linked to data on birth characteristics, the mother's ethnicity and race, and previously established risk factors. CMV deoxyribonucleic acid (DNA) detection in DBS was performed, followed by quantitative multiplex polymerase chain reaction (PCR). Neuroblastoma ras viral oncogene homolog (NRAS) was used to determine the quantity of genomic DNA, which was represented as picograms per PCR reaction.
Results
MBH found 1199 ALL-eligible patients and 4796 matched controls. The total sample consisted of 1189 cases along with 4756 controls. The average age upon diagnosis of ALL was 4.5 years. Participants were primarily born between 1993 and 2002, and there was a higher number of male children in the research sample. ALL cases had a greater mean birth weight than the controls. There were 153 cases with mothers aged 35 years or older compared to 547 controls.
The average pregnancy weight increase was comparable across mothers of both cases as well as controls. According to birth certificates, there were no considerable differences in mothers' smoking and alcohol consumption during pregnancy. The prevalence of pre-pregnancy or gestational diabetes was somewhat greater among mothers of cases, although this difference was not statistically significant. Among controls, the incidence of vaginal or uterine bleeding at the time of pregnancy was slightly higher than among case samples. Mode of delivery and number of births were comparable between cases and controls, with the majority of births occurring by spontaneous vaginal delivery. Furthermore, ALL patients had a considerably greater incidence of congenital abnormalities compared to controls.
Immunophenotype information was provided for 536 patients; including 62 T-cell ALL (T-ALL) and 474 B-cell ALL (B-ALL) patients. Those having immunophenotypes had a higher likelihood of being born after 1997 than those without them. Instances with subtype information were older at the time of diagnosis than cases without subtype information. Nonetheless, instances with and without subtypes were comparable across mother's ethnicity and race. There was available cytogenetic data for 127 B-ALL patients.
cCMV DNA was found in six of 1189 ALL patients and 21 of 4756 controls. ALL patients and controls had chances of cCMV infection that were not statistically different. In the multivariable model, there was no difference in the chances of cCMV exposure between cases and controls. Additionally, there were no T-ALL patients who tested positive for cCMV. Among individuals having subtype data who were positive for cCMV, there were two hyperdiploid instances. Due to the absence of exposure among the matched control individuals, the model did not converge when comparing CMV predominance among hyperdiploid ALL patients and their matched controls. In an unmatched study, hyperdiploid ALL patients had a 6.26 times higher likelihood of being CMV-positive than all controls.
Conclusion
The study findings of the present case-control research found no indication of a connection between pediatric ALL and cCMV infection. Nevertheless, the team discovered a correlation between hyperdiploid ALL instances utilizing modest sample sizes. The limited evidence provided here for the link between cCMV and ALL, as well as its growing biological plausibility, underscores the need for further investigation. Future research may potentially use DNA methylation to demonstrate a mechanistic relationship between ALL and cCMV.