Diabetic retinopathy (DR) is an ophthalmological complication of diabetes that is the primary cause of vision loss and blindness in this patient population.
DR is a frequent microangiopathic complication in Catalonia, Spain, with its incidence expected to increase due to the rise in diabetes, obesity, as well as an aging population. Therefore, nutritional therapy is integral to diabetes management and can help prevent late diabetes complications.
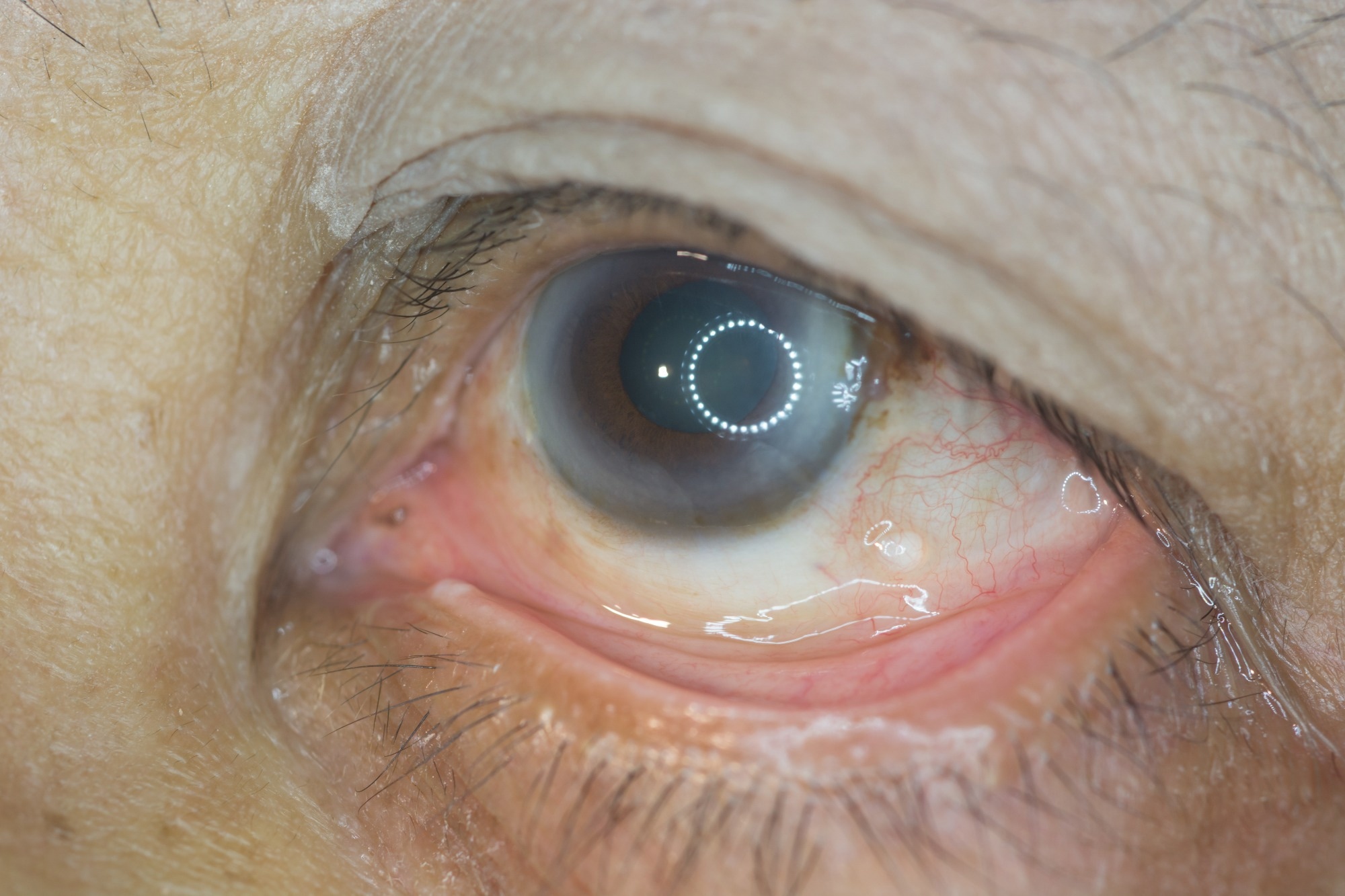
Study: Caffeine and the Risk of Diabetic Retinopathy in Type 2 Diabetes Mellitus: Findings from Clinical and Experimental Studies. Image Credit: ARZTSAMUI / Shutterstock.com
Caffeine and DR
Caffeine (1,3,7-trimethyl xanthine) is an active food component that is important for health. Among the primary sources of caffeine include tea, coffee, energy drinks, cola, chocolate, alcoholic beverages, and certain other food products such as gum.
Coffee is the richest source of caffeine taken daily by most of the general population worldwide. Many studies have reported that consuming between two and three cups of coffee can reduce the incidence of type 2 diabetes (T2D) and cardiovascular diseases.
However, a recent review indicated that the association between DR and caffeine remains unclear. For example, drinking more than two cups of coffee daily has been reported to be inversely correlated with DR prevalence among people with T2D.
Another study indicated that daily caffeine consumption could alter the retinal microvasculature in adults at an increased risk of cardiovascular issues, while a different study reported a protective effect of caffeine on the blood-retinal barrier in a cellular model of diabetic macular edema. However, few studies have also reported a neuroprotective effect of green tea on the retina of diabetic rats.
About the study
A new study in Nutrients discusses the relationship between caffeine intake and DR risk in people with T2D without any other late diabetic complications. It assesses the impact of caffeine using an experimental diabetic model.
The current study involved 144 T2D patients with DR and 147 people with T2D without DR. Recruitment of participants took place in the DR screening and treatment program at the University Hospital Arnau de Vilanova in Lleida, Spain, between March 2010 and January 2013. Information on the sex, age, self-reported ethnic group, physical activity, smoking habit, blood pressure, educational level, glycated hemoglobin (HbA1c), and antihypertensive and lipid-lowering drugs were obtained from all participants.
Data on antidiabetic treatments and diabetes duration were also obtained. Blood and urine samples were collected from all participants after fasting for 12 hours. A validated 101-item semiquantitative food frequency questionnaire (FFQ) was used to assess the usual intake of foods and nutrients, followed by a caffeine intake calculation.
In the experimental diabetic model, db/db male mice and non-diabetic control male mice (db/+) were subjected to caffeine or vehicle eye drops. Caffeine or vehicle eye drops were administered to the mice twice daily in each eye for two weeks.
After mice were euthanized, mouse retinas were stained for glial fibrillary acidic protein (GFAP) to assess the extent of neurovascular damage caused by either treatment. In addition, the Evans blue method was used to determine the permeability of the retinal vasculature by measuring the amount of albumin leaking from the retinas.
Study findings
Individuals with DR were older, had a larger waist circumference, higher frequency of hypertension, higher systolic blood pressure, higher glycated hemoglobin (HbA1c) levels, longer diabetes duration, more elevated high-density lipoprotein cholesterol (HDL-c) levels, and lower educational levels.
T2D patients who consumed the least amount of caffeine were more frequently affected by DR. However, no significant association was observed between coffee and tea consumption and the prevalence of DR. However, diabetes duration, HbA1c, and hypertension were associated with a greater risk of DR.
No difference in blood glucose concentrations and body weight was observed in db/db mice treated with caffeine compared to control mice.
Histological examination revealed that GFAP expression was confined to the retinal ganglion cell layer in non-diabetic mice compared to diabetic mice, which was expected. Notably, mice receiving caffeine did not exhibit any increase in GFAP expression, thus indicating that reactive gliosis did not increase as a result of caffeine exposure.
Non-diabetic mice exhibited less albumin leakage than diabetic mice treated with the vehicle. Although albumin leakage was lower in diabetic mice treated with caffeine than those treated with the vehicle, this difference was insignificant.
Conclusions
The study findings indicate that moderate and high caffeine intake offered protection against the development of DR among people with diabetes. Nevertheless, this difference was not replicated when comparing coffee and tea drinkers, which may be attributed to the different antioxidant compounds present in these drinks that may also offer some degree of protection against DR. Furthermore, the in vivo results from the current study did not indicate any effect of caffeine on the retina.
Further studies are needed to understand the possible benefits of caffeine intake and how other compounds found in tea and coffee may contribute to these effects. Additional research on the potential mechanisms responsible for the development of DR in people with T2D is also needed.
Limitations
The current study could not establish a relationship between caffeine intake and the development of DR. A second limitation was due to the small sample size in the human study. Finally, the presence of other compounds in caffeinated beverages was not analyzed.
Journal reference:
- Alcubierre, N., Granado-Casas, M., Bogdanov, P., et al. (2023). Caffeine and the Risk of Diabetic Retinopathy in Type 2 Diabetes Mellitus: Findings from Clinical and Experimental Studies. Nutrients. doi:10.3390/nu15051169.