In a recent study posted to bioRxiv* preprint server, researchers in Germany assessed the differences in antigen-specific immunoglobulin G (IgG) subtypes between post-COVID syndrome (PCS) patients and convalescent controls.
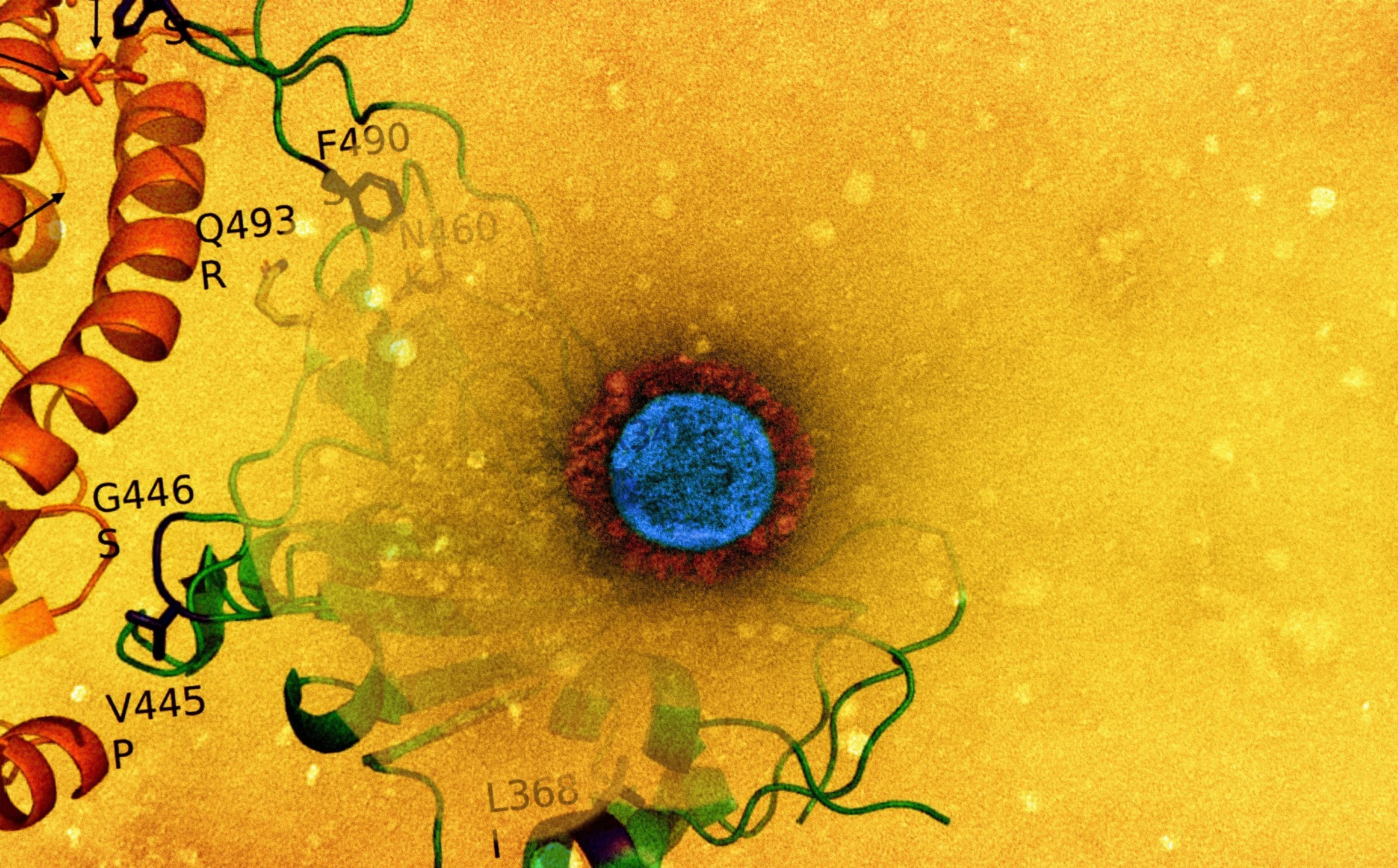 Study: IgG4 serum levels are not elevated in cases of Post-COVID syndrome. Image Credit: NIAID
Study: IgG4 serum levels are not elevated in cases of Post-COVID syndrome. Image Credit: NIAID

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Studies have demonstrated varying durability and levels of antibodies against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) after infection or vaccination. Effector functions are associated with four IgG subtypes (IgG1 – IgG4). In addition, two independent studies have reported elevated levels of IgG4 following the receipt of two or more mRNA vaccine doses, which is not observed with adenoviral vector vaccines.
IgG4 antibodies, which occur after prolonged antigen exposure, downregulate the immune response and induce tolerance. It was suggested that the protracted antigen availability in lymph node germinal centers after mRNA vaccination might increase IgG4 levels. Whether IgG4 antibodies are elicited after infection in non-vaccinated individuals remains unknown.
Further, persistent circulation of the viral antigen has been described for PCS patients. Increased class-switching of B cells to IgG4 may result in less fragment-crystallizable (Fc)-mediated effector function that may contribute to prolonged viral persistence and antigen circulation.
The study and findings
In the present study, researchers investigated whether PCS patients exhibit elevated IgG4 levels. Sixty-four PCS patients (44 females and 20 males) with a median age of 39.5 and 64 convalescent individuals (38 females and 26 males) with a median age of 37 were recruited. These subjects had been infected early in the COVID-19 pandemic when the Wuhan-like strain (D614G) and the Alpha variant were prevalent.
PCS patients and convalescent subjects were matched on age, sex, and the time from symptom onset to serum sampling. Ten PCS patients were vaccinated before sampling. Most PCS patients experienced fatigue (88%), dyspnea (81%), and memory/cognitive impairments (71%). Anti-spike antibodies of IgG subtypes were detected using a pre-fusion stabilized spike ectodomain-based enzyme-linked immunosorbent assay (ELISA).
The researchers observed differences in the levels of IgG subtypes. IgG1 was the most abundant antibody among subtypes, with median concentrations reaching 41.4 μg/ml for PCS subjects and 25.5 μg/ml for convalescent individuals. Both cohorts showed similar levels of IgG3 antibodies. Notably, the IgG4 concentrations were the lowest in both groups, with a median of 1.6 μg/ml.
A significant difference was observed in IgG2 levels between cohorts, with PCS patients showing lower concentrations. Further, the team assessed the reactivity of IgG4 antibodies against the spike protein, its receptor-binding domain (RBD), and the nucleocapsid protein’s C- (CTD) and N-terminal (NTD) domains.
There was a small but significant difference in the reactivity of IgG4 antibodies against RBD, but not for nucleocapsid or the spike protein. No biological relevance could be attributed to the differences, given the relatively low levels of IgG4.
Conclusions
The study provided insights into the distribution of SARS-CoV-2 spike-specific IgG subtypes in PCS patients and non-vaccinated convalescent individuals. The findings do not implicate IgG4 as a significant parameter in PCS development. Instead, low IgG2 levels may contribute to the long-term presence of SARS-CoV-2 antigens leading to chronic inflammation and lingering symptoms of the PCS.

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.