Forecasting future trajectories of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections, related hospitalizations, and deaths has been critical for making effective public health decisions. These forecasts can help hospitals anticipate surges in resource demands and policymakers/agencies distribute limited resources to high-risk areas.

Study: Forecasting the Trajectory of the COVID-19 Pandemic into 2023 under Plausible Variant and Intervention Scenarios: A Global Modelling Study. Image Credit: Mila Supinskaya Glaschenko / Shutterstock.com

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
About the study
In the present study, researchers created a susceptible-exposed-infectious (SEI) dynamic model to forecast COVID-19 trajectories for 2023 under various intervention and SARS-CoV-2 variant scenarios.
COVID-19 outcomes were predicted using a group of interlinked sub-models. The core model was the SEI transmission model that accounted for vaccination, multiple infections, antiviral therapies, and the waning of infection- and vaccine-induced immunity.
Using this model, the team first estimated historical infections, hospitalizations, and deaths by location, day, and variant. Much of this historical analysis was centered around the Omicron period spanning nearly 13 months from November 2021 to December 2022. The same outcome measures were assessed under five scenarios of new variant emergence for the period from December 12, 2022, to June 30, 2023.
In the baseline variant scenario, no new viral variant emerged. The remaining four scenarios had a few common features, including the same date of new variant emergence of January 15, 2023, South Africa as the place of emergence for new variant(s) identification, and following the Omicron invasion pattern, but differed in the parameterization of transmission severity and intensity. Of the remaining variant scenarios, the Omicron-like variant emerg,ed in one and a Delta-like variant appeared in the second.
The third model had an enhancement of the Delta-like scenario, whereas the final variant model (DeltaCron) was the worst-case scenario with the emergence of a variant with Omicron-like breakthrough capabilities and transmission intensity and Delta-like severity.
Finally, the team assessed the avertable COVID-19 burden with three intervention scenarios. These included increased mask usage, the reimposition of social distancing mandates, and variant-specific booster vaccine doses for all vaccinated subjects.
Study findings
According to the modeling projections, the SARS-CoV-2 Omicron variant was the predominant variant worldwide by November 27, 2021. The model estimated around 8.6 billion global SARS-CoV-2 infections between November 15, 2021, and December 12, 2022, with the Omicron and its sub-variants/lineages responsible for 8.47 billion infections. Most hospitalizations and deaths compared to infections during this period were attributable to the Delta variant.
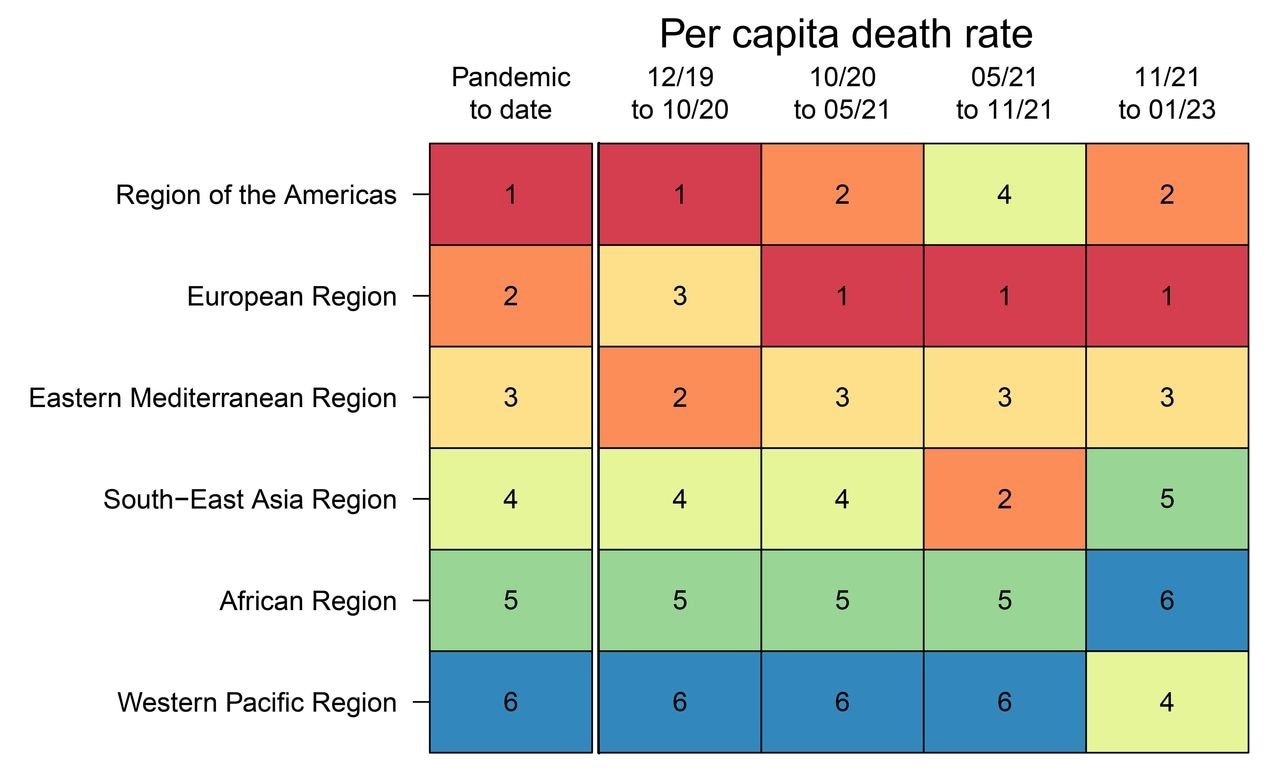
Per capita COVID-19 death rate ranking by WHO region. The far left “pandemic to date” column ranks the per capita death rate for each region for the entire pandemic up to December 12, 2022, by WHO region. This ranking determines relative ordering of WHO regions on the y-axis. The right four columns display relative rankings for four partitions of the pandemic, roughly corresponding to (a) pre-variant of concern phase, (b) Alpha, Beta, Gamma phase, (c) Delta phase, and (d) Omicron phase.
Almost all countries and territories experienced at least one Omicron wave. During the Omicron waves, Europe and the Americas had the highest per-person death rates, while South-East Asia and Western Pacific regions averted much of the severe outcome. The model estimated that 97.3% of the global population had been exposed to SARS-CoV-2 through vaccination, infection, or both, by December 12, 2022.
In the Western Pacific, much of their exposure was vaccine-derived due to the zero-COVID policy of China that ensured low infection rates. Conversely, Africa was primarily exposed to SARS-CoV-2 through infections due to limited vaccine availability/access. In the other regions, exposure was due to vaccination and infection.
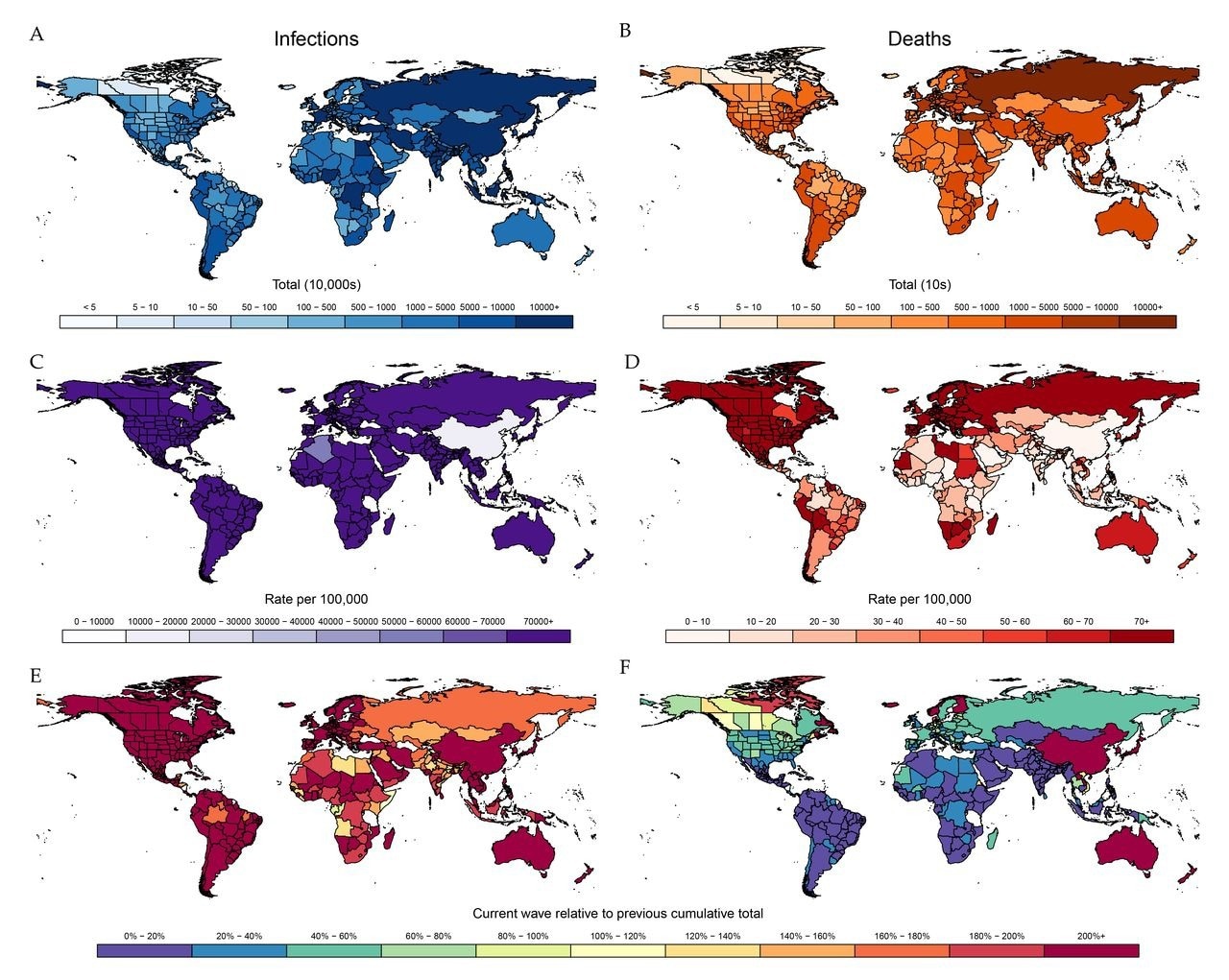
Cumulative total SARS-CoV-2 infections and COVID-19 deaths for Omicron wave from November 15, 2021, to December 12, 2022. Left column displays cumulative SARS-CoV-2 infections by location by count (A), rate (C), and relative size compared to entire pandemic up to November 15, 2021 (E). Corresponding values for COVID-19 deaths are shown in panels B, D, and F, respectively.
In the baseline variant scenario, the model projected 3.54 billion infections, 6.26 million hospitalizations, and 1.58 million deaths.
In the second variant scenario, an Omicron-like variant would have resulted in 5.19 billion infections, 13.6 million hospitalizations, and 2.74 million deaths, with over 2.6 billion cases attributable to this variant. A new variant with Delta-like characteristics would result in 3.64 billion infections, with the new variant accounting for only 423 million infections, 7.87 million hospitalizations, and 2.87 million deaths.
An enhanced Delta-like new variant would result in a massive COVID-19 burden, causing 4.5 billion infections, 21.3 million hospitalizations, and 11.1 million deaths. In the DeltaCron scenario, a new variant with Delta-like severity and Omicron-like infectivity would have resulted in the same number of infections as in the Omicron-like scenario but 30.2 million and 15.9 million hospitalizations and deaths, respectively.
Increasing mask usage to 80% of the population was postulated to prevent at least 15% of the predicted deaths across regions and variant scenarios. The social distancing mandate reimposition scenario would have only been mildly or moderately effective. In the variant-specific booster intervention scenario, the targeted booster had a minimal impact, with only a 3.2% reduction in global COVID-19 mortality.
Combining the mask use and mandate reimposition scenarios would have averted up to 36% of estimated COVID-19 deaths by June 2023. This joint intervention scenario would have prevented 5.44 million deaths in the DeltaCron scenario and a minimum of 19% of estimated deaths across all regions and variant scenarios.
Conclusions
The researchers of the current study explored different scenarios that reflected the potential emergence of new SARS-CoV-2 variants under several interventional approaches. Expedited variant-specific vaccine boosters had little impact, regardless of the transmissibility and severity of existing and future variants.
Notably, increasing mask usage was associated with substantial reductions in infections and mortality rates, whereas mandate reimposition mildly/moderately reduced future COVID-19 burden. Combining these two interventions led to an even more significant impact than individually. Above all, the analysis showed that simple interventions, including masking and social distancing mandates, could be critical tools against COVID-19.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.