Neuroplasticity is the ability of neuronal circuits to reorganize and adapt to the changing environment. Research efforts have long focused on identifying mechanisms within the brain underlying neuroplasticity, but a growing body of evidence suggests that endogenous signals from the periphery may also be involved. The gut microbiota is one such example that can influence human physiology.
Like other senses, information is transmitted between the brain and the microbiota. The microbiota-gut-brain axis is a complex signaling network involving chemical transmitters, neuronal pathways, and the immune system. This axis might be central in modulating brain-related processes, such as myelination, neural plasticity, and microglia maturation, influencing complex behaviors. The present study summarized how gut microbiota could influence behavior and neuroplasticity.
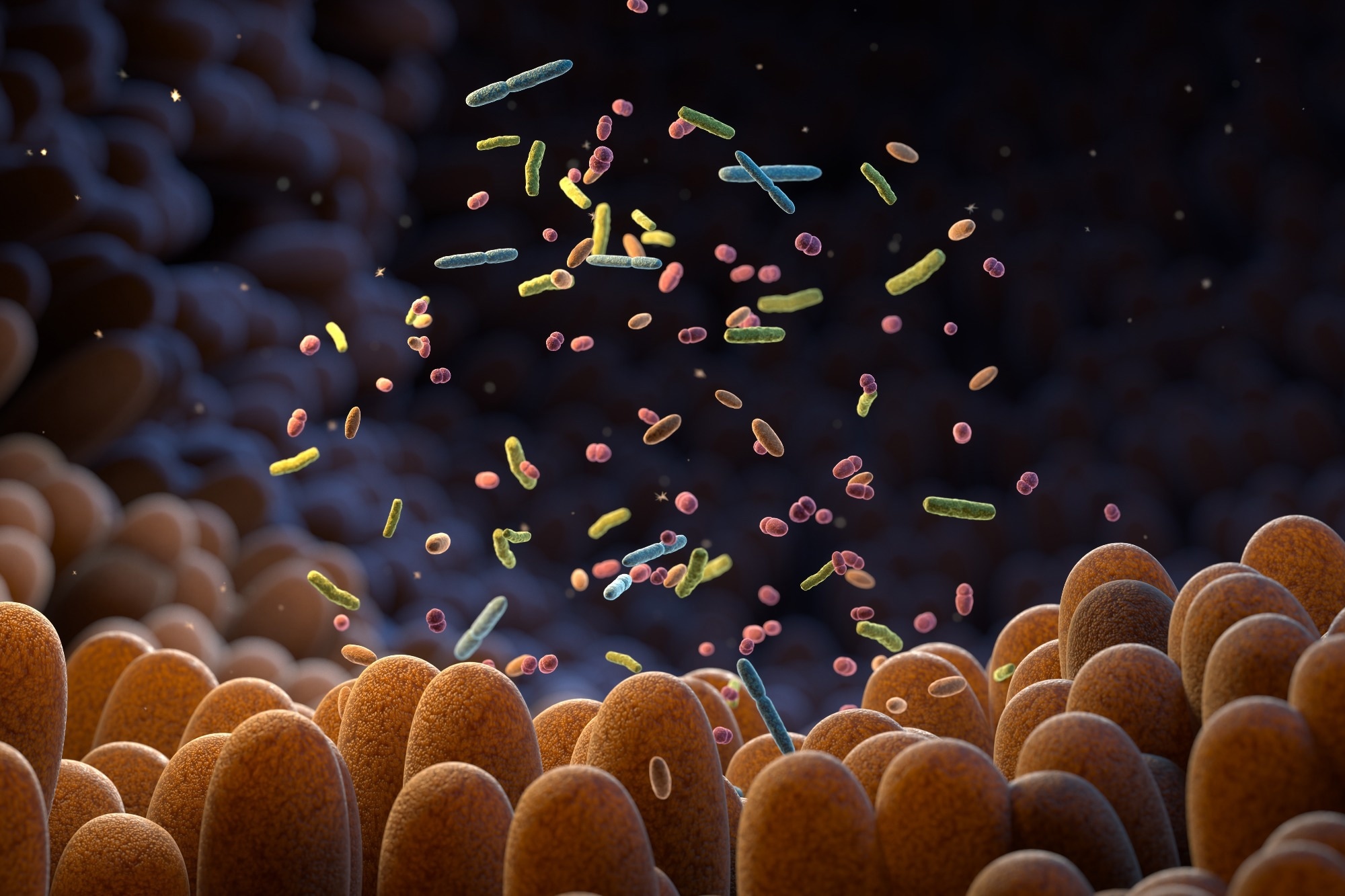 Study: The gut-brain connection: Exploring the influence of the gut microbiota on neuroplasticity and neurodevelopmental disorders. Image Credit: Tatiana Shepeleva / Shutterstock
Study: The gut-brain connection: Exploring the influence of the gut microbiota on neuroplasticity and neurodevelopmental disorders. Image Credit: Tatiana Shepeleva / Shutterstock
Gene expression regulation by microbiota
Short-chain fatty acids (SCFAs) are metabolites mainly synthesized by the microbial fermentation of dietary fibers in the colon. These metabolites have been reported as inhibitors of histone deacetylase (HDAC). SCFAs can promote histone acetylation allowing transcription factors to bind to DNA and activate transcription.
A study demonstrated that gut bacteria influence histone acetylation, and administering SCFAs to germ-free (GF) mice could recapitulate epigenetic reprogramming driven by the microbiota. Another study revealed that SCFAs impact gene expression in primary cortical astrocytes; intriguingly, genes involved in neuroplasticity mechanisms were among the upregulated transcripts.
DNA methylation is another epigenetic mark involved in neuronal plasticity. DNA methylation changes occur while learning and memory formation; its involvement has been demonstrated in experience-dependent plasticity. While commensals in the intestine can induce DNA methylation changes in the epithelial cells, microbiota-driven action on the transcription/methylation of the DNA in the brain is not yet established.
Regulation of neuroactive agents
Gut microbes provide different metabolites that act as essential neuroactive molecules. Intestinal bacteria can synthesize neurotransmitters, such as histamine, dopamine, tryptophan, γ-aminobutyric acid (GABA), serotonin, and their precursors (acetate, choline, tyrosine). The blood-brain barrier (BBB) is impermeable to large molecules, such as neurotransmitters, which are produced from their precursors within the brain.
The ability of gut bacteria to produce precursors that may reach the brain suggests a potential role in influencing cognitive function and behavior through neuroplasticity. Only 10% of the serotonin is synthesized in the brain, and the majority is produced in the gastrointestinal (GI) tract. While changes in serotonin synthesis in the GI tract are unlikely to impact the central nervous system (CNS), some evidence indicates that gut microbiota might influence brain serotonin.
Although microbiota-dependent brain plasticity modulation through changes in GABA has not been observed, microbiota-derived GABA may indirectly modulate brain function through the vagus nerve or by acting on the enteric nervous system. Moreover, bacteria-derived acetate has been shown to modulate GABA levels in the hypothalamus.
Effects on the microglia
In a study, microbiota exhibited an altered morphology and immature transcriptomic signature in the absence of gut microbiota, which was rescued after SCFA administration. Further, the gut microbiota affects the density and shape of dendritic spines. Lately, a study in GF zebrafish observed that impaired social behavior was associated with less precise targeting of neurons in the forebrain and decreased neurite complexity.
This was associated with alterations in microglial cell numbers and the expression of the complement cascade, suggesting that microbiota might modulate processes related to structural plasticity and behavior by influencing microglial actions on synapses. In addition, gut microbiota might impact adult neuronal circuits via microglial cells.
Microbiota actions on neuroplasticity during development
Several studies report the potential existence of microbes in the placenta and amniotic fluid and that microbial colonization of the GI tract might commence during gestation. Since colonization coincides with CNS maturation, the postnatal period might serve as a window for the microbiome to shape brain development. Neuronal circuits are highly plastic and susceptible to exogenous influences during this period.
For example, the normalization of the exaggerated stress response in young GF mice was achieved by the fecal transplantation of microbes from specific pathogen-free (SPF) mice only at an early stage of development. Depleting microbes from weaning SPF mice also impaired cognitive, emotional, and social behavior, suggesting that the microbiome can impact brain function and behavior.
Neurodevelopmental disorders
Neurodevelopmental disorders are characterized by brain development/function impairments, leading to motor, emotional, and cognitive deficits. Some examples include schizophrenia, autism spectrum disorder (ASD), Rett syndrome (RTT), cyclin-dependent kinase-like 5 (CDKL5) deficiency disorder, and attention deficit hyperactivity disorder (ADHD).
Besides neuropsychiatric conditions in ASD, autistic persons may have higher risks of comorbidities, such as GI dysfunctions, pro-inflammatory responses, diabetes, obesity, and immune abnormalities. GI disturbances in ASD could be associated with dysbiosis. Data from the literature indicates a substantial inter-individual heterogeneity in microbes affected in ASD.
Nonetheless, an increase in Clostridium species and Firmicutes and a decrease in Bacteroidetes have been consistently observed in ASD patients. Non-invasive interventions such as probiotics, prebiotics, dietary changes, and antibiotics have improved ASD symptoms in patients and mouse models. Like ASD patients, many patients with RTT experience GI problems, and reduced gut microbial diversity has been observed in RTT patients.
Concluding remarks
The general consensus is that gut microbiota plays a role in metabolism and immunity. While it is difficult to establish the interactions between the brain and the intestine, several other pathways facilitate crosstalk between them. There is some consensus on the ability of gut microbiota to influence behavior and neuroplasticity. Future research on neuroplasticity and neuronal function may shed light on inexplicable issues.