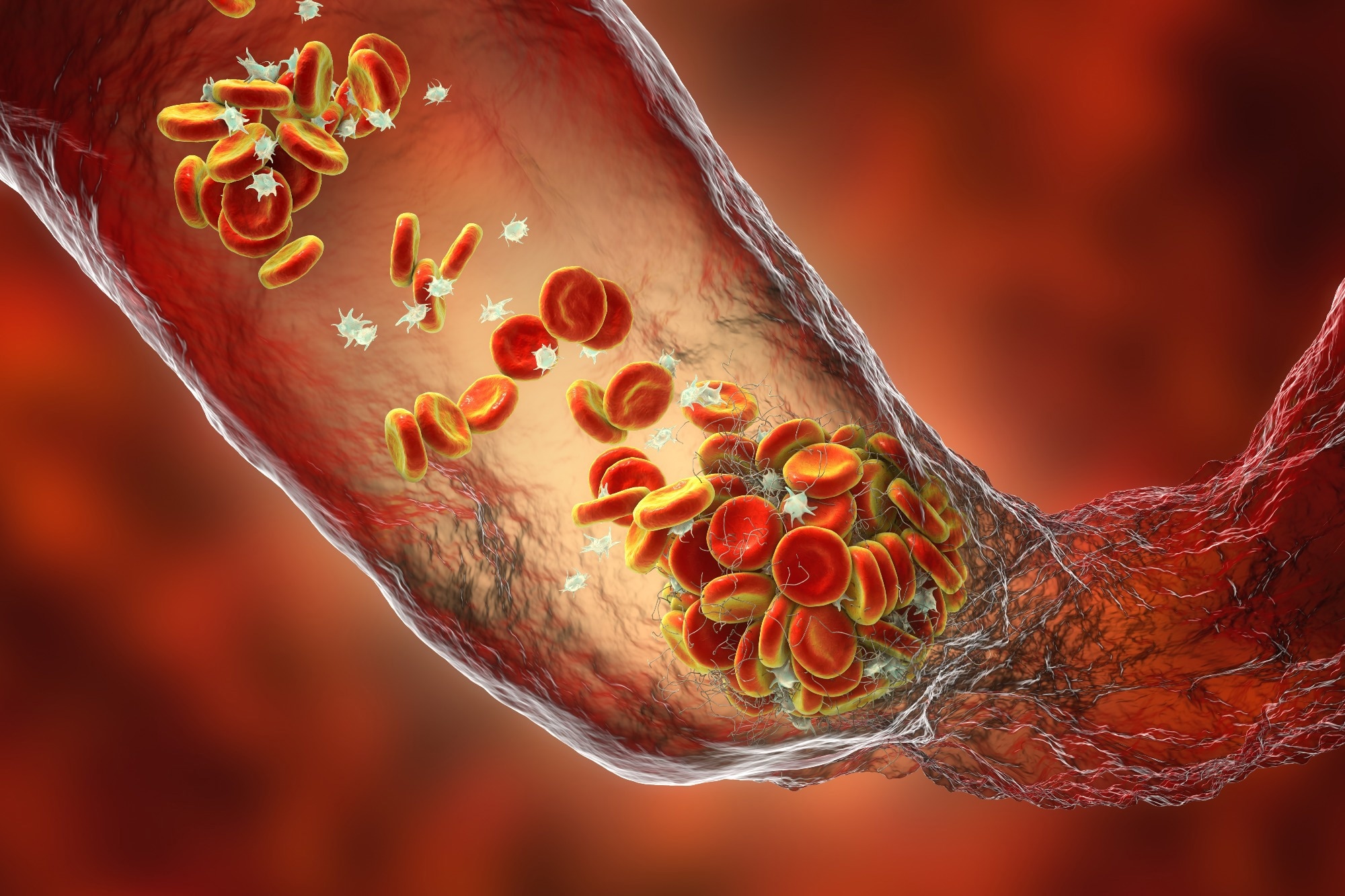
 Study: Effect of Thromboprophylaxis on Clinical Outcomes After COVID-19 Hospitalization. Image Credit: Kateryna Kon / Shutterstock
Study: Effect of Thromboprophylaxis on Clinical Outcomes After COVID-19 Hospitalization. Image Credit: Kateryna Kon / Shutterstock
Background
Several studies have shown that patients hospitalized due to an acute severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, especially those requiring care in an intensive care unit (ICU), were at an increased risk for arterial and venous thromboembolism (VTE). Studies have also found that microvascular thrombosis might be a risk factor for post-acute sequelae of COVID-19 (PASC) at a later time point.
Depending on the illness severity, doctors give anticoagulant therapy to such patients to prevent thromboembolic complications during the hospital stay.
However, studies have documented that thromboembolic events might occur even after hospital discharge, though at variable frequencies. Thus, an extended course of thromboprophylaxis after hospital discharge might benefit some patients. However, data favoring the same is scarce.
About the study
In the present study, researchers determined whether a prolonged course of anticoagulant therapy from the day of hospital discharge to 30 days would reduce the frequency of thromboembolism events and mortality among adults hospitalized for COVID-19 but discharged after 48 hours or more.
More specifically, this double-blind, placebo-controlled trial included 18 years or older participants hospitalized for COVID-19 for two or more days and ready for discharge. The team compared the efficacy and safety of clinically available antithrombotic strategies in these patients.
In addition, they assessed health-related quality of life (QoL) using the EuroQol-5D (EQ-5D) questionnaire to investigate whether extended thromboprophylaxis would affect PASC development.
It provides a single index measure of QoL by assessing health across five domains, mobility, self-care, day-to-day activities, discomfort or pain, and anxiety and depression. A maximum score of one indicates the best health state per the EQ-5D questionnaire.
In stage one of this protocol, the researchers randomly assigned study participants to apixaban, an anticoagulant therapy, and placebo groups, with individuals in the former group receiving two doses of 2.5 mg of apixaban daily, the latter a matching placebo.
All the participants received a 30-day supply of the drug or placebo before hospital discharge. They continued post-discharge follow-up visits for 90 days, using telephonic or e-mail surveys.
Through rigorous follow-ups on days two, 10, 20, 30, 45, and 90, the researchers ensured medication/placebo initiation and adherence. Moreover, they assessed clinical outcomes in response to the therapy, including the incidence of thromboembolic complications after the extended course of the anticoagulant therapy.
The primary endpoint of this study encompassed all-cause mortality and venous and arterial thromboembolic events; examples include pulmonary embolism and myocardial infarction within 30 days. The secondary endpoints covered all the primary endpoints at days 45 and 90 of follow-up.
Results
Between February 2021 and June 2022, the team randomly assigned 610 and 607 participants from 107 US hospitals to apixaban and placebo groups, respectively. Unfortunately, on 23 June 2022, they had to terminate the study enrollment.
The trial was interrupted early because of an unexpected decline in COVID-19 hospitalizations in the US and a subsequent decline in thromboembolic events. Consequently, the study was inconclusive and fetched indefinite results.
In the placebo-treated participants, the study estimated primary endpoint rate was 4% by day 30 after hospital discharge. The composite primary outcome rates were even lower, i.e., 2.3%, suggesting that the increased risk for thromboembolic events during hospitalization was not so distinct post-discharge.
The results for the primary composite endpoint of arterial thromboembolism, VTE, or all-cause mortality were highly comparable for apixaban and placebo groups. Accordingly, the authors noted that these events occurred in 13 and 14 participants of the apixaban and placebo groups, respectively.
The authors noted comparable results concerning secondary endpoint and safety outcomes. Overall, 105 participants reported 137 serious adverse events, and 54 (8.9%) and 51 (8.4%) participants from the apixaban and placebo groups reported at least one serious adverse event, respectively. Furthermore, the median EQ-5D index scores were comparable between the apixaban and placebo groups at days 30 and 90, i.e., 0.93 and 0.94 at day 30 and day 90 for both groups, respectively.
Conclusion
The study was inconclusive, yet, its results for the primary composite endpoint of VTE, arterial thromboembolism, and all-cause mortality at 30 days were highly similar for therapy and placebo groups. The efficacy estimates for the primary composite endpoint ranged between a 56% reduction and a 95% increase in risk across the apixaban and placebo groups.
Journal reference:
- Wang, T.Y., Wahed, A.S., Morris, A., Kreuziger, L.B., Quigley, J.G., Lamas, G.A., Weissman, A.J., Lopez-Sendon, J., Knudson, M.M., Siegal, D.M. and Kasthuri, R.S., 2023. Effect of thromboprophylaxis on clinical outcomes after COVID-19 hospitalization. Annals of Internal Medicine, DOI: https://doi.org/10.7326/M22-3350, https://www.acpjournals.org/doi/10.7326/M22-3350