Cardiovascular disease (CVD) is the primary cause of death worldwide and, as a result, poses a significant challenge for patients, clinicians, and researchers. CVD encompasses various diseases that affect the heart, blood vessels, and blood.
Nanomedicine is an exciting field that aims to improve patient outcomes through transformative treatments, imaging agents, and ex vivo diagnostics. In a recent study published in the journal Nature Cardiovascular Research, researchers review recent advancements in nanomedicine treatment options for CVD.
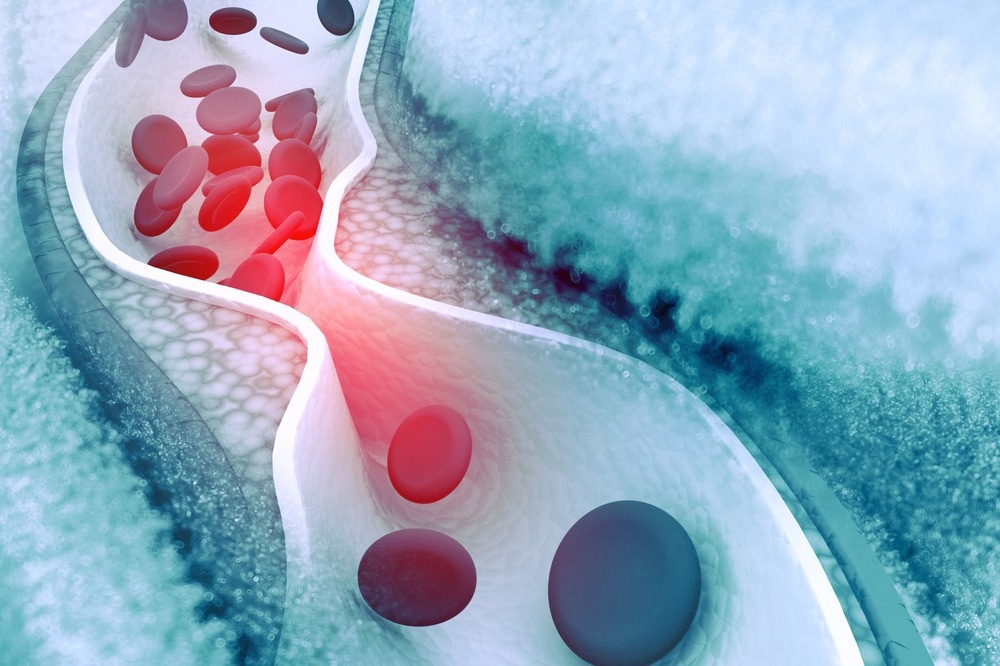
Study: Nanomedicines for cardiovascular disease. Image Credit: hywards / Shutterstock.com
Cardiovascular nanoimmunotherapy
Cancer immunotherapy has advanced significantly; however, CVD immunotherapy remains in its early stages. Targeting the innate immune system can have significant risks, including compromising natural defenses and increasing the risk of infection and sepsis.
Various nanotherapies have been created to specifically target phagocytic macrophages and inflammatory monocytes (iMos) that are known for their ability to take up nanomaterials and subsequently contribute to inflammation and disease development. These cells can also initiate immune responses, monitor trained immunity, and naturally migrate to areas of inflammation like atherosclerotic plaques.
Nanomaterials have the potential to deliver therapeutics that can inhibit macrophage and monocyte proliferation and trafficking, activate and polarize helper T-cells, trigger cholesterol efflux, and boost apoptosis. Taken together, these processes can help facilitate the anti-inflammatory resolution of atherosclerotic plaques, as well as the physiological factors associated with other CVDs.
Various studies have utilized myeloid-targeting ligands or cellular phagocytosis to selectively target nanomaterials and increase sensitivity to ultimately limit the potentially negative effects of these agents. Nanomaterial libraries can also be screened in vivo to improve immune cell selectivity.
Nanoimaging
Various types of nanomaterials, including magnetic, acoustic, optical, and nuclear nanomaterials, are used in preclinical CVD nanoimaging, specifically for the detection of atherosclerosis. Nanomaterials can create signal contrast that matches their cognate imaging modality. For example, magnetic iron oxide nanomaterials are used for magnetic resonance imaging (MRI) and myocardial perfusion imaging (MPI), while gold nanomaterials can be used for computed tomography (CT) imaging.
Nanomaterials have limited molecular targets associated with CVD pathogenesis as compared to normal tissues due to a reduced number of molecular mechanisms that have been implicated in CVD. Nevertheless, CVD imaging can be used to identify a high prevalence of diverse populations when an effective imaging target is detected, which is in contrast to cancer that may not have the same level of prevalence.
Ex vivo diagnostics
Nanomaterials can enhance the detection of cellular and molecular biomarkers associated with CVD, such as troponins and C-reactive protein (CRP), by utilizing their physicochemical and magnetic properties to amplify signals and increase sensitivity during imaging. Furthermore, nanomaterials can enhance the CRP signal by modulating various properties such as electrical, optical, electrochemical, and chemiluminescent characteristics.
Multiplexable plasmonics can be used to estimate hypertension-related blood autoantibodies and microalbuminuria in urine, which can indicate endothelial or vascular dysfunction. Metallic nanomaterials and quantum dots have been used in electrochemical methods to detect cardiac biomarkers such as troponin, CRP, creatine kinase, and myoglobin. These methods involve voltammetry, amperometry, and impedance spectroscopy to sense analytes through direct electron transfer.
Radiology, liquid, and pathology biopsy evaluations are often separated in clinical practice, which can result in inadequate integration and suboptimal treatment choices. As a result, the full value of multiple tests used in screening, diagnosis, therapeutic dosage optimization, patient stratification, and response to therapy evaluation may not be fully realized.
Artificial intelligence (AI) could be used to identify both in vivo and ex vivo biomarkers that reflect a specific disease state, determine the most effective therapy or combination of therapies, and interpret the results of therapeutic responses, even among various patient subpopulations.
Nanomaterials can enhance multiplexing for ex vivo diagnostics and in vivo multicolor molecular imaging. This can improve the accuracy and sensitivity of these processes without significantly increasing their associated time or costs. Such approaches can also help researchers select the best biomarker sets to examine using new nanodiagnostic methods in a standardized way.