The patient was ineligible for an allograft and needed veno-arterial extracorporeal membrane oxygenation support due to a deteriorating heart condition.
The donor pig had ten modified genes and passed all screening methods employed in non-human primate (NHP) experiments.
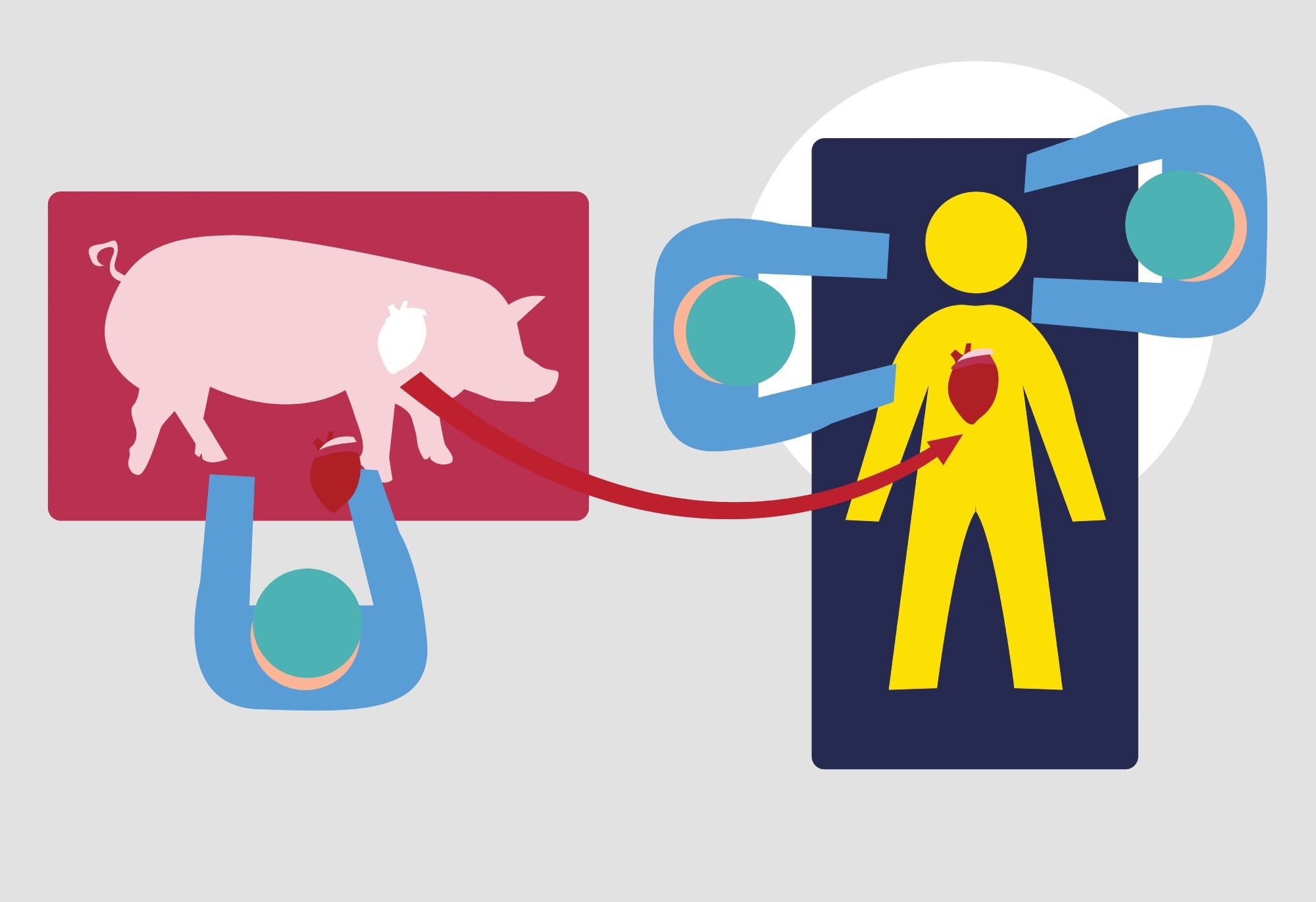 Study: Graft dysfunction in compassionate use of genetically engineered pig-to-human cardiac xenotransplantation: a case report. Image Credit: CrystalEyeStudio/Shutterstock.com
Study: Graft dysfunction in compassionate use of genetically engineered pig-to-human cardiac xenotransplantation: a case report. Image Credit: CrystalEyeStudio/Shutterstock.com
About the study
In the present study, researchers extensively monitored the patient in an intensive care unit (ICU) to gather all physiological and biochemical parameters critical for caring for all heart transplant recipients.
Additionally, they performed deoxyribonucleic acid (DNA) polymerase chain reaction (PCR) and ribonucleic acid (RNA) transcription for extensive immunological and histopathological studies, including electron microscopy (EM) and quantification of porcine cytomegalovirus or porcine roseolovirus (PCMV/PRV) in the xenograft and recipient's cells and tissues.
Furthermore, the researchers performed intravenous immunoglobulin (IVIG) binding to donor cells and single-cell RNA sequencing of peripheral blood mononuclear cells (PBMCs).
Results
After successful xenotransplantation surgery, till postoperative day 47, the patient was hemodynamically stable; his graft functioned well on echocardiography and performed cardiovascular and other functions. Then, xenograft quickly became oedematous, and the patient suffered diastolic heart failure.
The endomyocardial biopsy on postoperative day 50 uncovered that fluid and red blood cells (RBCs) accumulated with few inflammatory cells in the interstitial space. Then, by day 56, fibrotic tissue replaced the interstitial edema over time, leading to rare thrombotic microangiopathy and complement deposition.
EM investigations showed that the myocardial capillary bed and nearby myocardial cells suffered endothelial cell injury that caused degenerative changes in these cells, including loss of myofilaments. The doctors could not understand the reason for such extensive damage. The examination of post-mortem specimens did not detect an intact virus.
Together, these events deteriorated the patient's condition. So, with his family's consent, doctors withdrew support, and subsequently, the patient died from graft failure on day 60 after surgery.
It is noteworthy that in this patient, because of his pancytopenia and increased likelihood of contracting recurrent infections, researchers had to reduce immunosuppression.
He had significant amounts of B and T lymphocytes in the mediastinal lymph node after two days of immunosuppression therapy, indicating incomplete induction; yet, the results of B-cell phenotyping were inaccurate because of interference by plasma cells and few circulating B cells.
In non-NHP models, mycophenolate mofetil is a key component of immunosuppression. Its use completely ceased in this patient between postoperative days 20 and 54.
Instead, the doctors gave tacrolimus to the patient, and, as in NHP studies, it could not ineffectively prevent graft rejection. It also likely contributed to pig xenoantibody-mediated endothelial cell damage.
In NHP studies, researchers have demonstrated that a high dose of 2C10R4 adequately suppresses B-cell function, preventing the emergence of anti-graft antibodies.
Since the minimum efficacious KPL-404 dose in humans in transplant settings is unknown, the researchers attempted to deliver its highest concentration to this patient while accounting for extrinsic factors.
However, several factors reduced the bioavailability of this therapeutic antibody to its target. First, increased inflammatory response or target-mediated drug disposition increased the drug dose needed to sustain its therapeutic levels in this patient.
Second, extrinsic factors played a role; examples include plasmapheresis and IVIG binding to endothelial cells, which prevented the Fc binding of KPL-404.
Further, the authors noted higher levels of anti-pig IgGs in this patient post-IVIG administration for severe hypogammaglobulinemia. There is evidence that IVIG is beneficial in allotransplantation. So, the researchers tested three different commercially available IVIGs with aortic endothelial cells from the donor pig heart.
However, the observation that the patient's serum had high concentrations of anti-pig IgG and its increased binding on immunohistochemistry suggested an exogenous IgG source.
It confirmed that the role of anti-pig antibodies in IVIG therapy triggered endothelial damage, which might be more significant in xenotransplantation than in allotransplantation. Thus, it needs further investigation in future studies.
Furthermore, the authors considered the likelihood of xenoantibody-mediated rejection. Due to reduced immunosuppression drug levels in the recipient, the authors noted endothelial injury and low C4d deposition in the first and limited thrombi in the last biopsy.
The authors emphasized that the critical role of the complement pathway cannot be overlooked, despite protective genes, e.g., hCD47, hCD46, hDAF presence, and C1 esterase inhibition.
So, they performed a few complement assays to accurately interpret the complement pathway's role in xenotransplantation and its rejection. However, due to a lack of tissue availability and proper controls, these assays could not fetch convincing results about the autologous role of C3.
Thus, future experiments should thoroughly evaluate the role of complement pathways in xenotransplantation cases.
The pig was positive for PCMV/PRV DNA, and the authors also detected PCMV/PRV DNA in the transplanted xenograft; however, no tissue from the patient had an actively transcribing virus.
Most likely, PCMV/PRV DNAemia resulted from circulating (or lysed) xenograft cells from PCMV/PRV virions made in the xenograft, not the patient organs. Despite the evidence of PCMV/PRV DNAemia, the researchers observed no cytopathic changes in the heart on EM.
Nonetheless, EM data revealed the reactivation of latent PCMV/PRV virus in the pig heart. Likely, immune suppression initiated extensive cell lysis-triggered endothelial injury. Also, an assessment of the myocardium demonstrated gradual damage and capillary bed loss.
Conclusions
In this case report, researchers identified potential mediators of the observed endothelial injury. They also found evidence that reactivation and replication of latent PCMV/PRV in the xenograft initiated a lethal inflammatory response. These results pointed to specific measures to improve xenotransplant outcomes in the future.
Thus, the researchers concluded that a genetically engineered porcine heart and anti-CD40-based therapy could keep a xenotransplant recipient alive for up to 60 days.
However, more pig-to-human transplantation studies could improve the understanding of mechanisms governing xenograft failures in humans to inform better management of clinical xenotransplantation.