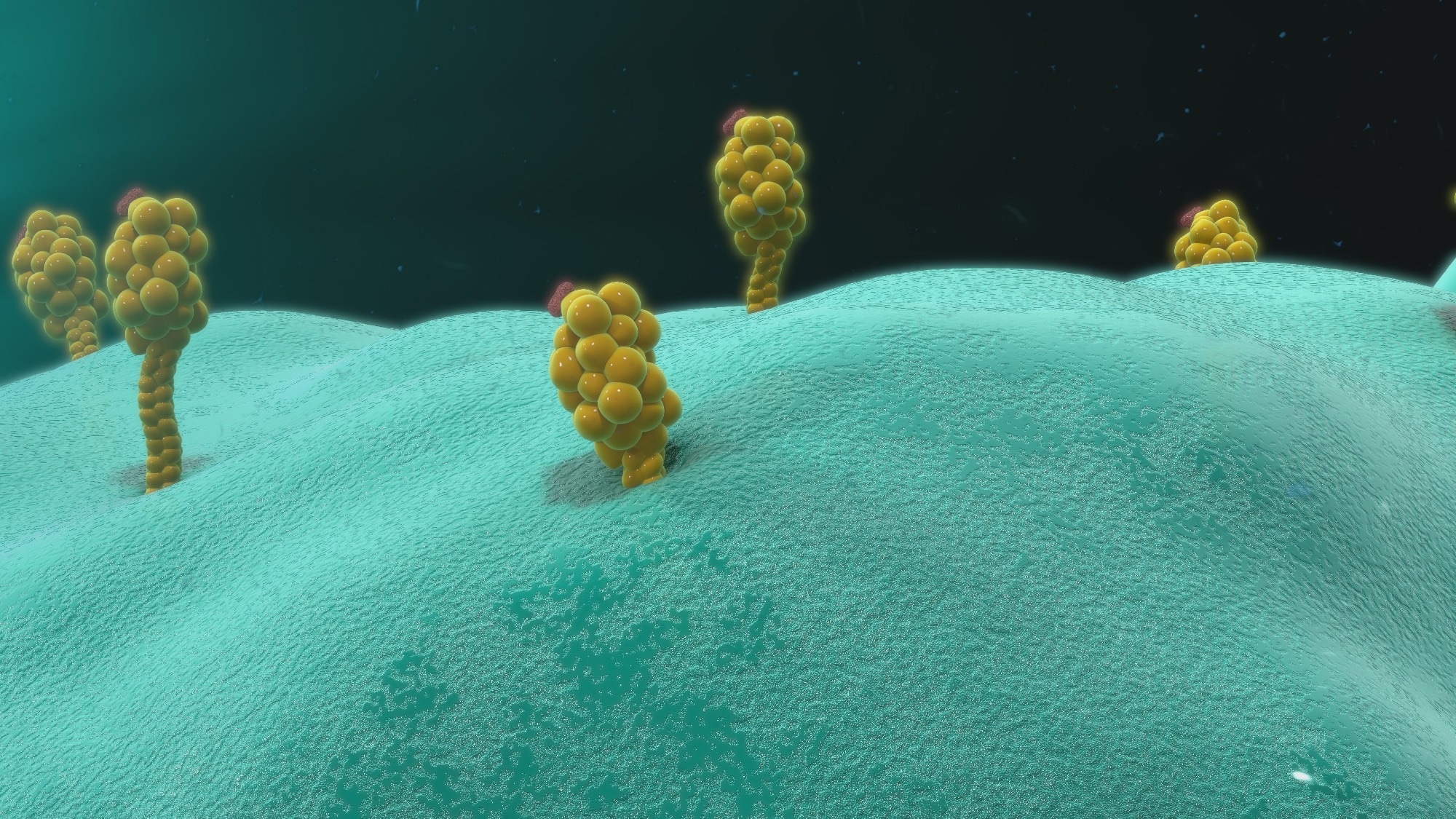
 Study: A common allele of HLA is associated with asymptomatic SARS-CoV-2 infection. Image Credit: sciencepics/Shutterstock.com
Study: A common allele of HLA is associated with asymptomatic SARS-CoV-2 infection. Image Credit: sciencepics/Shutterstock.com
Background
Numerous studies intending to understand the genetic basis of differential outcomes in COVID-19 have examined genetic associations with severe disease course, primarily in hospitalized cohorts, e.g., the multicentre Host Genetics Initiative.
However, few studies have examined genetics in non-hospitalized, prospective, community-based cohorts. Studies directly examining HLA associations with infection had relatively small cohorts and fetched mixed and inconclusive results.
Hundreds of genes govern human immune responses to diseases, of which HLA variants have the most robust associations with viral infections. It makes them relevant molecular targets for COVID-19 vaccine development.
Individuals expressing HLA-B*46:01 might be more vulnerable to COVID-19. Conversely, HLA-B*15:03 protects against COVID-19 by presenting highly conserved SARS-CoV-2 peptides to T cells.
More in-depth insights into the impact of HLA variation(s) in infectious diseases could inform vaccine development and potential immunotherapies for COVID-19.
About the study
The present study had a smartphone-based study design which helped the researchers track COVID-19 symptoms and outcomes, including positive reverse transcription-polymerase chain reaction (RT-PCR) test results of nearly 30,000 individuals previously HLA genotyped for five loci, HLA-A, -B, -C, -DRB1 and -DQB1.
Notably, they included positive test result data till 30 April 2021 from people who self-identified as belonging to the 'white' ethnicity. They retrieved their data from a pre-existing database for medical research named the National Marrow Donor Program (NMDP).
Further, they contextualized the study results by examining T cell reactivity, T cell receptor (TCR) repertoire, affinity, and structural implications for the observed HLA associations.
Furthermore, the researchers examined the crystal structures of the HLA-B*15:01 molecule in a complex with peptides from other seasonal coronaviruses (CoVs), e.g., HKU1-CoV and OC43-CoV, at concentrations of five μM and ten μM.
Results
The main study finding was that the HLA-B*15:01 allele was markedly associated with asymptomatic infection in participants reporting a SARS-CoV-2-positive test result.
Nearly 10% of individuals with European ancestry carry this common allele and remain asymptomatic post-SARS-CoV-2 infection than those who do not.
Another important effect of HLA-B*15:01 homozygosity was that it increased the likelihood of remaining asymptomatic during SARS-CoV-2 infection by >eight times. Asymptomatic patients in two independent cohorts of the study also had highly similar frequency distributions of HLA-B*15:01.
Furthermore, the study results showed that the HLA-DRB1*04:01 allele augmented the HLA-B*15:01 effect when paired, like in the United States (US)-origin people who self-identified as white.
Upon analyzing immunodominant epitopes in T cells in human peripheral blood mononuclear cells or PBMCs from pre-pandemic healthy donors, the authors observed that the cells from donors carrying HLA-B*15:01 allele unexposed to SARS-CoV-2 were reactive to the SARS-CoV-2 spike (S) peptide NQK-Q8, and most cells displayed a memory phenotype.
Thus, this amino acid sequence identity between seasonal CoVs and SARS-CoV-2 S peptides explains the T cell cross-reactivity.
The presence of high-affinity, cross-reactive memory T cells in unexposed donors further corroborated the robust association between the allele HLA-B*15:01 and asymptomatic COVID-19.
Other recent studies have also shown that SARS-CoV-2-specific memory T cells are enriched at the site of infection and help rapidly clear the overt onset of symptoms by secreting more interferon-gamma (IFN-Ύ).
S peptides from SARS-CoV-2 and other CoVs, namely NQK-Q8 and NQK-A8, showed comparably stabilized the HLA-B*15:01 molecule. Also, HLA-B*15:01 presented these peptides in similar structural conformation, which gives a molecular basis to pre-existing immunity and T-cell cross-reactivity.
More importantly, despite limited data on HLA-B*15:01 epitopes found in SARS-CoV-2 patients, this study's results found NQK-Q8 as the prime candidate peptide governing HLA-B*15:01-mediated T cell cross-immunity with seasonal CoVs.
Conclusions
The study results strongly support the role of the HLA-B*15:01 allele in mediating asymptomatic COVID-19 through pre-existing T-cell immunity due to previous exposure to other CoVs.
The understanding that HLA class I alleles play a crucial role in early infection and the mechanisms underlying early viral clearance leading to asymptomatic SARS-CoV-2 infection have important implications.
It becomes the framework for future studies refining vaccine development and therapies for early disease.