Within the renin-angiotensin system (RAS), which regulates blood volume, electrolyte balance, and systemic vascular resistance within the body, the angiotensin-converting enzyme 2 (ACE2) cleaves angiotensin II (Ang II) to Ang-(1-7), which subsequently leads to vasodilation. Under normal physiological conditions, ACE2 expression can be found within the thymus, lungs, kidneys, pancreas, and heart.
In a recent study published in the Journal of Biomedical Science, researchers describe the role of ACE2 in chronic diseases, such as cardiovascular diseases (CVDs), diabetes, and coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
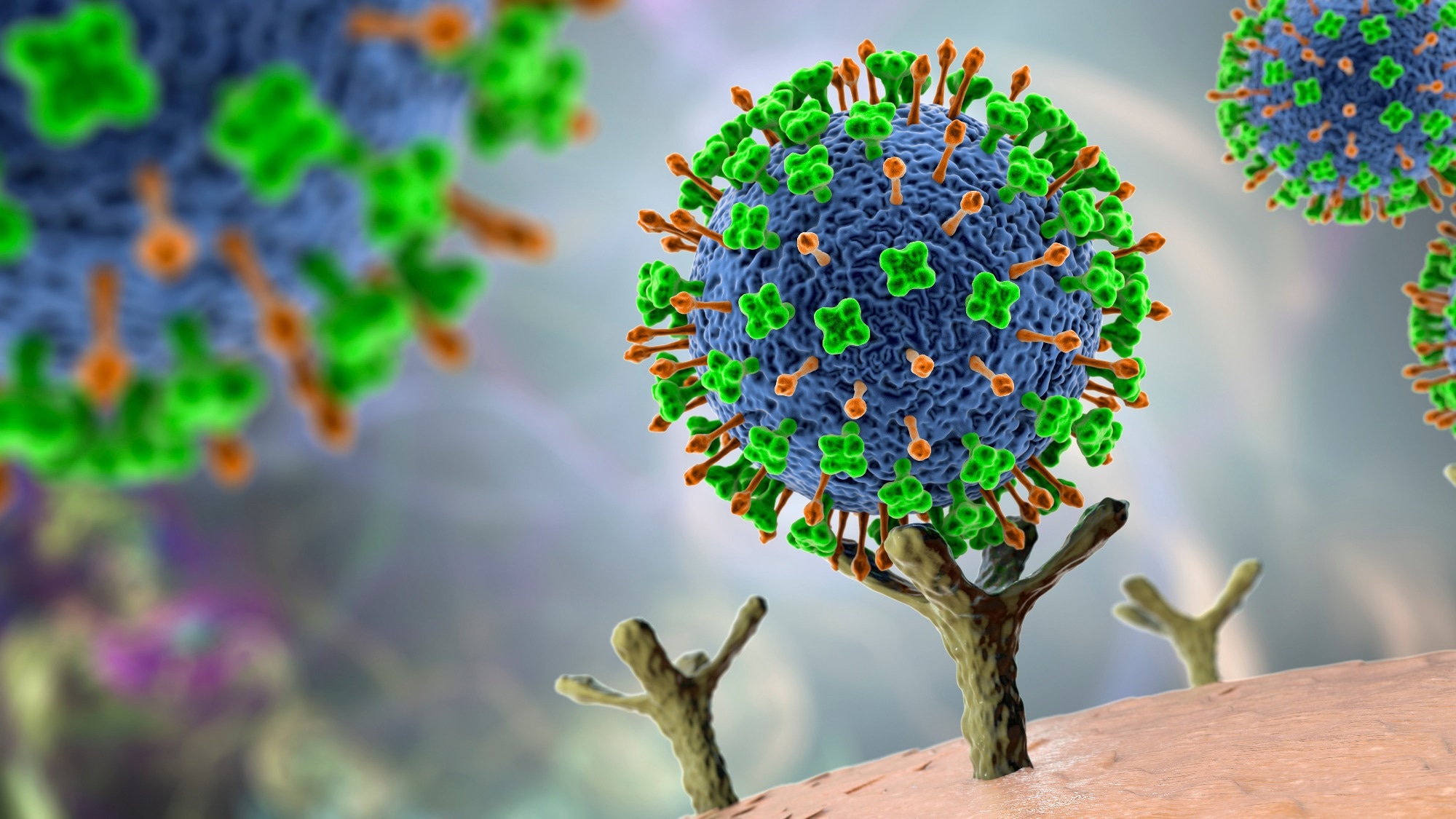 Study: ACE2 in chronic disease and COVID-19: gene regulation and post-translational modification. Image Credit: Kateryna Kon / Shutterstock.com
Study: ACE2 in chronic disease and COVID-19: gene regulation and post-translational modification. Image Credit: Kateryna Kon / Shutterstock.com
The role of ACE2 in chronic diseases
Within endothelial cells, RAS regulates vasodilation, antifibrosis, and antihypertrophy, all of which prevent the development of pulmonary hypertension, with ACE2 levels inversely correlated with pulmonary arterial pressure (PAP) levels. Likewise, lungs and artery endothelial cells from pulmonary arterial hypertension (PAH) patients often exhibit reduced ACE2 levels.
Certain environmental factors may also impact ACE2 levels, as demonstrated by significantly reduced ACE2 protein levels observed in lung epithelial cells following exposure to cigarette smoke extract (CSE) and benzo(a) pyrene (BaP), the latter of which is a known carcinogen. Notably, the reduced expression of ACE2 in smokers may limit the cellular entry of SARS-CoV-2, thus suggesting that the infection efficiency of this virus is lower in smokers. Nevertheless, tobacco use has been shown to increase the risk of severe COVID-19.
Despite the loss of its C-terminal tail following cleavage by a disintegrin and metalloprotease 17 (ADAM17), soluble ACE2 (sACE2) has been implicated in various disease processes. For example, increased levels of sACE2 have been reported in the urine from both type 1 and type 2 diabetes patients, as well as diabetic mice, with sACE2 urinary levels also correlated with severe diabetic kidney disease. Increased levels of sACE2 and ADAM17 have also been identified in blood samples obtained from patients with heart failure due to myocardial infarction.
Regulating ACE2 expression in COVID-19
To gain entry into cells for infection, the SARS-CoV-2 spike protein attaches to ACE2 receptors present on the surface of host cells. SARS-CoV-2 has been shown to upregulate the expression of ACE2, with severe COVID-19 patients often exhibiting high plasma levels of ACE2.
Since the onset of the COVID-19 pandemic, researchers worldwide have investigated potential therapeutic approaches that can prevent infection with SARS-CoV-2 by directly targeting viral proteins, ACE2, and other up- and downstream molecules that may be involved in this process.
For example, previous studies have shown that the overexpression of ACE2 during SARS-CoV-2 infection can be mitigated by the knockdown of ubiquitin carboxyl-terminal hydrolase L1 (UCHL1). In fact, the inhibition of UCHL1 by the LDN-5744 inhibitor successfully prevented SARS-CoV-2 infection in clinically relevant human cell lines, thus indicating that UCHL1 inhibitors may mitigate SARS-CoV-2 infection by downregulating the expression of ACE2.
Vitamin C supplementation has also been shown to reduce the effects of COVID-19. This antiviral activity is likely due to the inhibition of ubiquitin-specific peptidase 50 (USP50), whose overexpression mediates the stabilizing deubiquitination of ACE2 proteins. Thus, vitamin C ultimately reduces the expression of ACE2 proteins, thereby limiting SARS-CoV-2 entry into cells.
Glycosylation, which involves the conjugation of glycan chains to a protein on different residues of the ACE2 protein, is directly involved in COVID-19. For example, glycosylation of the ACE2 at the Asn90 site prevents the SARS-CoV-2 spike protein from successfully binding to the cellular receptor. Comparatively, altered glycosylation of ACE2 ASN90 and Thr92 residues increase the binding affinity of ACE2 to the viral spike protein.
Study takeaways
The ACE2 protein is widely expressed throughout the body; therefore, its appropriate expression is crucial for normal physiological functions. The reduced expression of ACE2 in vascular endothelial cells, artery smooth muscle cells, cardiomyocytes, renal tubular epithelial cells, and pancreatic islet cells has been documented in various chronic diseases.
During COVID-19, cellular ACE2 surface receptors are crucial for successful infection. As a result, ACE2 can be used as both a biomarker of disease severity and a target for pharmacotherapeutics.
Thus, future agents capable of increasing the expression of ACE2 through agonists positive regulators of ACE2 or inhibiting repressor molecules can be used to prevent infection or treat chronic diseases.
Journal reference:
- Wang, C. W., Chuang, H. C. & Tan, T. H. (2023). ACE2 in chronic disease and COVID-19: gene regulation and post-translational modification. Journal of Biomedical Sciences 30(71). doi:10.1186/s12929-023-00965-9