The amphiregulin (AREG)–epidermal growth factor receptor (EGFR) axis mediates this interaction at the molecular level.
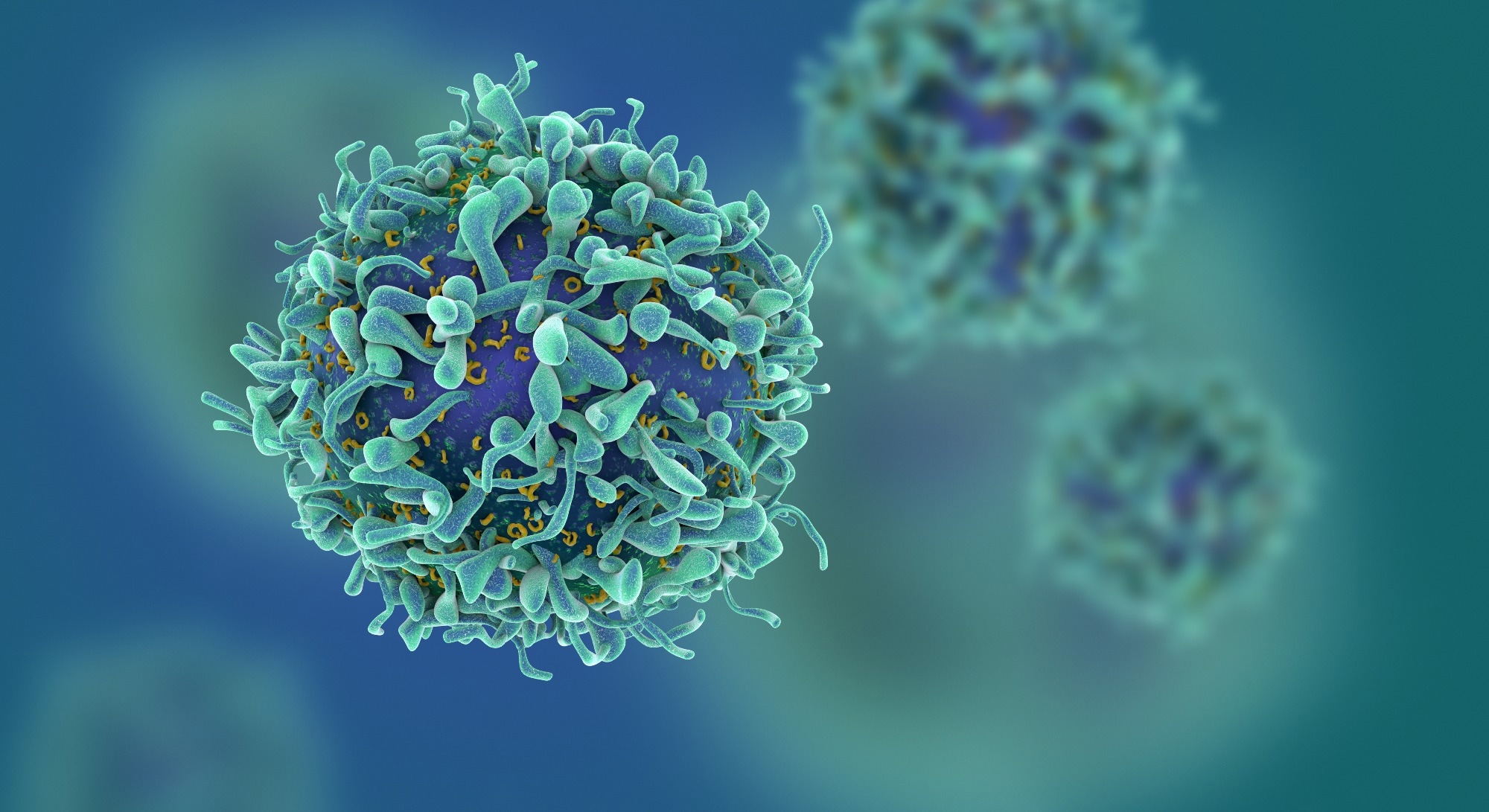 Study: Amphiregulin couples IL1RL1+ regulatory T cells and cancer-associated fibroblasts to impede antitumor immunity. Image Credit: fusebulb/Shutterstock.com
Study: Amphiregulin couples IL1RL1+ regulatory T cells and cancer-associated fibroblasts to impede antitumor immunity. Image Credit: fusebulb/Shutterstock.com
Background
Under normal physiological conditions, several cells, including epithelial cells, endothelial cells, and fibroblasts, constitutively express an inactive form of the cytokine interleukin-33 (IL-33).
In case of tissue damage due to an environmental insult, tumor growth, or other diseases (e.g., asthma), IL-33 ('alarmin') alerts several target immune cells expressing IL1RL1 (ST2), which initiates a cascade of immunological and pathological processes.
Besides CAFs, IL-33 alerts many other immune cells, including mast cells, macrophages, basophils, eosinophils, dendritic cells, type 1/2 T cells, and Treg cells.
However, the effect of IL-33 on CAFs is of special interest as it likely helps these immune cells suppress immune responses by promoting IL1RL1+ Treg cell accumulation.
In other words, IL-33 enhances the Tregs-CAFs crosstalk via the AREG–EGFR axis, leading to immune suppression in the tumor microenvironment (TME).
AREG activates EGFR to promote the expression of tumor-growth factor-beta (TGF-β) in CAFs, which likely causes immunosuppression in the TME. Notably, EGFR expression is predominant in CAFs but not Treg cells and other cell types in the TME. However, the precise mechanisms used by IL1RL1+ Treg cells to alter the TME and promote tumorigenesis are still elusive.
Furthermore, recent studies have shown that IL-33 potentially inhibits tumor progression by enhancing the immune type I responses.
In addition, IL-33, in combination with immune checkpoint inhibitors, facilitates mounting an additive immune response against tumors. Thus, understanding the precise role of the cytokine IL-33 in cancer could help researchers develop novel cancer immunotherapies.
About the study
In the present study, researchers used a transplant murine model of a lab-engineered B16 melanoma cell line overexpressing B16–IL-33, a secreted form of IL-33, to examine how IL-33 shapes the T-cell immune responses within the TME.
They performed paired single-cell ribonucleic acid sequencing (scRNA-seq) and T-cell receptor sequencing (TCR-seq) of TCR-β+ T cells to analyze the immune cellular network in B16 and B16–IL-33 tumors on day nine post-tumor inoculation.
It helped them evaluate the impact of IL1RL1 signaling in Treg cells and examine the involvement of the AREG/EGFR axis in Treg cell-CAFs crosstalk within the TME and its significance in IL-33-mediated antitumor immunity.
Further, the researchers analyzed clonal expansion using paired scTCR-seq data. Additionally, they used flow cytometry (FC) to confirm the study findings using another transplant mouse model of MC38 colon carcinoma.
Finally, the team used single-cell regulatory network inference and clustering (SCENIC) to identify transcription factors (TFs) and their target genes, which together are termed regulons, which program IL1RL1+ Tregs and CD8+ T cells in B16–IL-33 and B16 tumors.
Results
The study data comprised 11,022 cells of three T-cell lineages: conventional T (Tconv) cells, cluster of differentiation (CD)4+ Treg cells, and CD8+ T cells. B16–IL-33 versus B16 tumors showed increased Treg and CD8+ T cells and decreased Tconv cells accumulation.
There are six clusters of CD8+ tumor-infiltrating lymphocytes (TILs), and IL-33 led to a marked change in compositions of each. FC analysis showed that overexpression of IL-33 in tumor cells markedly increased the percentage of interferon-gamma (IFN-γ)+ CD8+ T cells in the TME.
The paired scTCR-seq revealed that naïve CD8+ TILs comprised single TCR clones in B16 and B16–IL-33 tumors. In the remaining five clusters, B16–IL-33 tumors had a higher percentage of clonally expanded CD8+ TILs with a larger clonal size, indicating that IL-33 also increased the clonal diversity of CD8+ TILs.
scRNA-seq analysis of Tregs from B16–IL-33 tumors showed that IL1RL1-deficient Tregs had reduced accumulation compared to control Tregs, with increased accumulation of pre-effector (pre)Tregs and effector €Tregs, suggesting that IL1RL1 is necessary for the accumulation of IL1RL1+ Tregs in tumors. The regulons with the highest activities in IL1RL1+ Treg cells were Bcl3 and nuclear factor κB-2 (Nfkb2).
Of three major CAF subtypes, antigen-presenting (ap)CAFs highly expressed major histocompatibility complex II (MHCII) antigen presentation pathway, which likely engaged and stimulated Treg cells in the TME.
Thus, treatment with anti-AREG antibodies inhibited tumor growth and improved overall survival in B16–IL-33 tumor-bearing mice.
Conclusions
Overall, the study data supported that IL1RL1+ Treg cells exert a pro-tumor function through the AREG/EGFR-mediated interaction with CAFs within the TME.
Further, it demonstrated that AREG helped couple IL1RL1+ Treg cells to CAFs, thereby restricting the antitumor efficacy of IL-33. These findings could inform the development of new immunotherapies for cancer.