In a recent study published in The Lancet Respiratory Medicine, researchers evaluated the burden and determinants of multiorgan abnormalities following hospitalization due to moderate to severe cases of coronavirus disease 2019 (COVID-19) and their associations with disease outcomes.
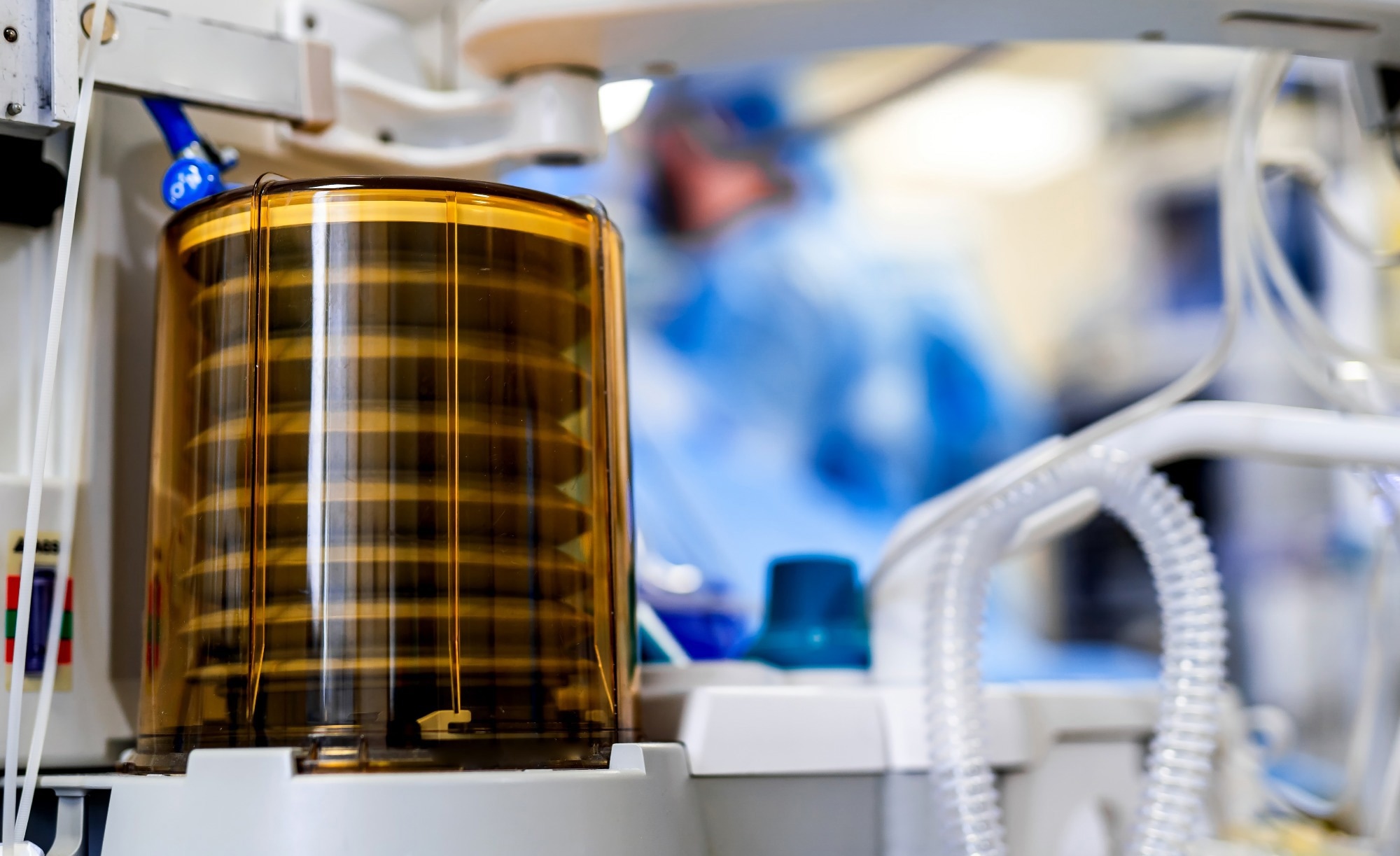 Study: Multiorgan MRI findings after hospitalisation with COVID-19 in the UK (C-MORE): a prospective, multicentre, observational cohort study. Image Credit: Terelyuk / Shutterstock
Study: Multiorgan MRI findings after hospitalisation with COVID-19 in the UK (C-MORE): a prospective, multicentre, observational cohort study. Image Credit: Terelyuk / Shutterstock
Background
A large body of evidence suggests that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections result in long-term multiorgan complications, and potential causes include viral cytotoxicity, ischemic injury, chronic inflammation, metabolic derangements, and the impact of treatment methods such as invasive ventilation. This multitude of persistent symptoms, such as chronic fatigue, dyspnea, post-exertional malaise, and gastrointestinal and neurological complications, is now referred to as post-acute sequelae of COVID-19 (PASC) or long coronavirus disease (long COVID).
However, while many studies have explored potential mechanisms of long COVID, the burden of the multiorgan impairments that persist after hospitalization due to COVID-19 and their impact on the outcomes and recovery of patients remains unclear. In this respect, magnetic resonance imaging (MRI) is an excellent tool to assess the organ manifestations that occur after moderate to severe SARS-CoV-2 infections, with previous studies reporting an association between inflammatory markers and abnormal findings in tissues, as well as alterations in hemostatic pathways.
About the study
In the present study, the researchers conducted a multicenter, multiorgan MRI follow-up across the United Kingdom (U.K.) of patients who had been hospitalized with COVID-19. This study, called Capturing Multiorgan Effects of COVID-19 or C-MORE, was designed to characterize and evaluate the prevalence of multiorgan impairments in patients who had recovered from COVID-19 as compared to individuals who had never been infected with SARS-CoV-2.
C-MORE also aimed to decipher the possible mechanisms of COVID-19-related multiorgan dysfunction and examine whether these multiorgan abnormalities were associated with the outcomes reported by the patients. Patients hospitalized with polymerase chain reaction (PCR)-confirmed or clinically diagnosed SARS-CoV-2 infections between March 2020 and November 2021 were enrolled in this prospective, observational study.
As part of the follow-up, clinical evaluations, including lung function tests and blood sampling, were conducted. MRI scans were acquired for the heart, lungs, brain, kidneys, and liver. Individuals above the age of 18, with no contraindications on the MRI, who had not been hospitalized in the last year, and who were asymptomatic for recent or previous COVID-19 with negative nucleocapsid antibody and PCR tests were invited to serve as controls on the study.
Clinical and demographic characteristics, comorbidities, the clinical progression scale as specified by the World Health Organization, and the area of residence were recorded for all the participants. Individuals with MRI contraindications such as metal or other implants, including pacemakers or defibrillators, and claustrophobia were excluded from the study.
Blood and pulmonary function tests were also conducted for all the participants, with forced expiratory volume, forced vital capacity, and, in some cases, carbon monoxide transfer factor in the lung being measured to assess pulmonary function. Outcome measures related to anxiety, cognitive function, dyspnea, and fatigue were assessed using various questionnaires.
Results
The findings suggested that hospitalization due to COVID-19 increased the medium-term risk of multiorgan abnormalities. The MRI results reported a higher incidence of multiorgan abnormalities in post-hospitalized COVID-19 patients as compared to healthy controls, with more frequent findings of lung, brain, and kidney abnormalities among the COVID-19 patients. However, the frequencies of liver and cardiac MRI abnormalities were similar for the patients and controls. Hemostatic or vascular and inflammatory injury patterns were also observed for some organs on the MRI.
Furthermore, the presence of multiorgan abnormalities was found to be linked to age, with individuals who were marginally older, with more than three comorbidities, and who had experienced a more severe form of SARS-CoV-2 infection exhibiting a higher incidence of multiorgan abnormalities.
The assessment of outcome measures reported by the patients also indicated that abnormal MRI findings in the lungs were associated with twice the risk of chest tightness, and multiorgan abnormalities on the MRI were associated with severe and persistent mental and physical health impairments following hospitalization with COVID-19.
Conclusions
Overall, the findings reported that multiorgan MRI abnormalities on the MRI were three times more prevalent among patients who had been hospitalized with COVID-19 as compared to uninfected, healthy individuals. The MRI revealed hemostatic and inflammatory injury patterns in some organs, and the multiorgan abnormalities were linked to persistent and severe mental and physical impairments. These results highlight the need for multidisciplinary therapeutic and management strategies for post-hospitalized COVID-19 patients.
Journal reference:
- K, B. J., Lone, N. I., Jones, S., Shaw, A., Hairsine, B., Kurasz, C., Henson, H., Armstrong, L., Shenton, L., Dobson, H., Dell, A., Lucey, A., Price, A., Storrie, A., Pennington, C., Price, C., Mallison, G., Willis, G., Nassa, H., & Haworth, J. (n.d.). Multiorgan MRI findings after hospitalisation with COVID-19 in the U.K. (C-MORE): a prospective, multicentre, observational cohort study. The Lancet Respiratory Medicine. https://doi.org/10.1016/S22132600(23)00262X, https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(23)00262-X/fulltext