They examined Alpha, Delta, Beta, Gamma, and Omicron VOCs, all independently evolved from an early lineage wave 1 (W1) SARS-CoV-2 strain. Beta and Gamma spread in limited geographical regions, whereas Alpha, Delta, and Omicron BA.1 spread worldwide.
Expectedly, their sustained human-to-human transmission required evasion from human's (host) innate and adaptive immunity, wherein several selective forces came into play to drive evolution.
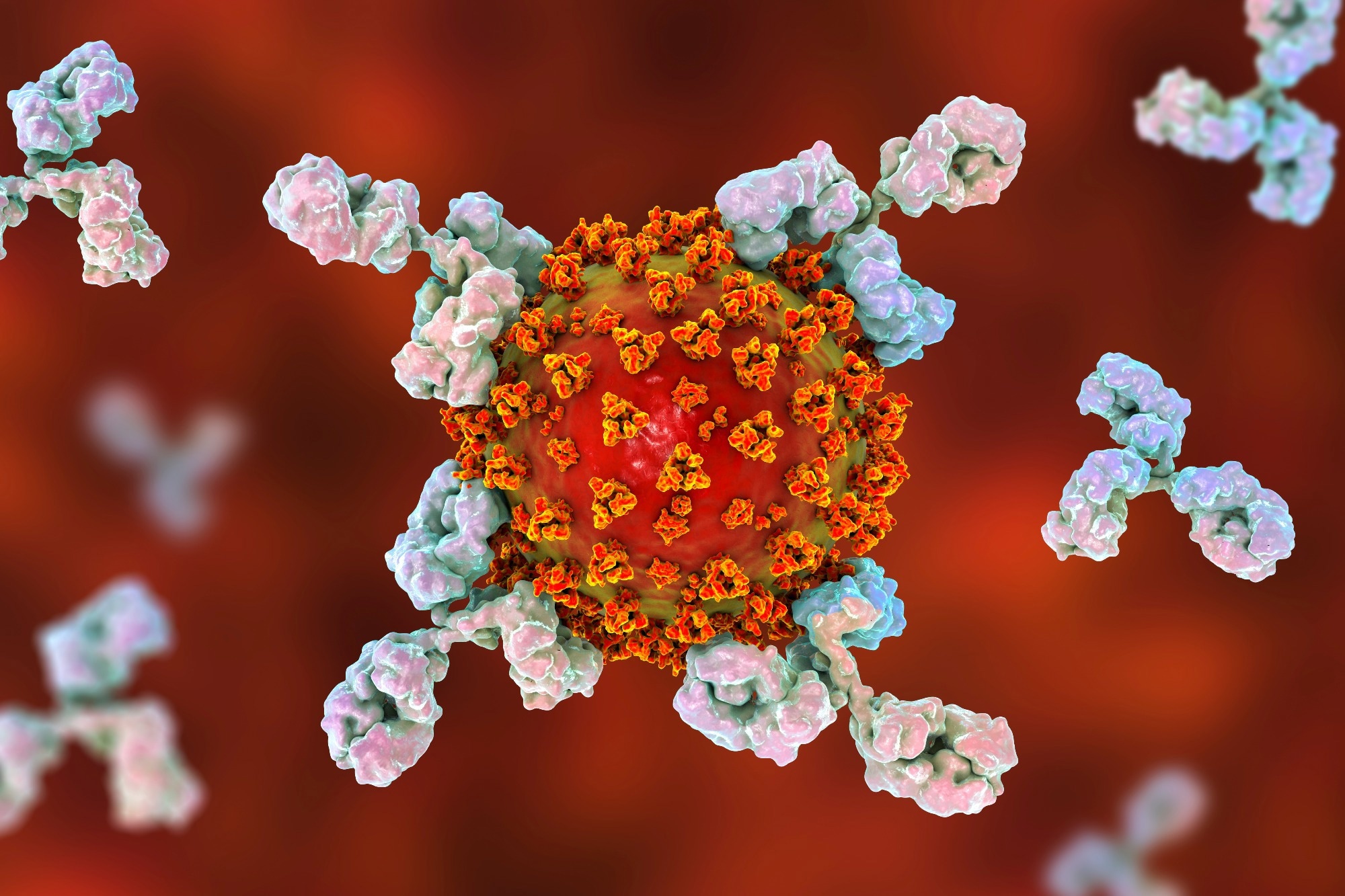 Study: SARS-CoV-2 variants evolve convergent strategies to remodel the host response. Image Credit: Kateryna Kon / Shutterstock
Study: SARS-CoV-2 variants evolve convergent strategies to remodel the host response. Image Credit: Kateryna Kon / Shutterstock
Background
Previous studies have extensively examined the most mutated SARS-CoV-2 spike (S) glycoprotein. However, VOCs have acquired additional non-synonymous mutations in non-structural proteins, NSP3/6/9/12/13, nucleocapsid (N), membrane (M), and envelope (E) structural proteins, and several open reading frames (ORFs), Orf3a/6/7a/8/9b.
Researchers found that these mutations (outside of S) also modulate the host response to infection; however, the impact of those mutations, especially non-coding mutations across VOCs, remains poorly understood.
About the study
In the present study, researchers first collected SARS-CoV-2 VOCs-infected Calu-3 cells at 10 and 24 hours post-infection (hpi) for bulk messenger ribonucleic acid sequencing (mRNA-seq), mass spectrometry (MS) abundance proteomics, and phosphoproteomics analysis.
They quantified genome levels of viral stocks by quantitative reverse transcription-polymerase chain reaction (qRT-PCR), not plaque assays, to equalize input doses across all VOCs. Thus, except for Omicron BA.1, W1 viruses and all VOCs displayed equivalent replication kinetics, which the team also compared in air-liquid-differentiated primary human airway epithelial (HAE) cells.
Additionally, they performed affinity purification-MS (AP-MS) on ectopically overexpressed VOCs and W1 proteins to define changes in virus-host protein interactions. Further, the team quantified viral subgenomic RNA (sgRNA) and protein level differences for each virus during replication in Calu-3 cells.
Results
The study data suggested that all VOCs independently evolved from the W1 virus but later enhanced the same set of viral proteins using three convergent molecular strategies.
First, they altered viral gene expression during infection; secondly, all, except Gamma, modulated viral protein phosphorylation, notably on the N protein, which likely affected viral assembly or replication. Finally, all accumulated protein-coding mutations altered virus-host protein interactions. Specifically, the novel VOC-specific protein N* interacted with the host RNA polymerase II (RNAPII)-associated factor (PAF) complex (PAFc), suggesting VOCs evolved to influence the host gene expression through N*.
Comparing VOCs with W1 viruses uncovered 16% of changes in virus-host interactions. The proteomic analysis found that each sample had 58-62k unique peptides and 23–35k modulated phosphorylation, corresponding to 4,800–5,100 and 3,700–4,300 unique proteins, respectively. Most alterations/mutations occurred at phosphorylation (57%) levels, followed by RNA levels (38%), while protein abundance showed minimal changes (7%).
An increase in global RNA expression and protein levels decreased at 24 hpi, likely suggesting the induction of the inflammatory response to the virus at the translational level during infection. Phosphorylation levels were bi-directional, indicating their complex signaling during infection.
One of the most striking features of SARS-CoV-2 VOCs was their ability to sequentially replace one dominant strain, e.g., the Delta VOC replacing Alpha, and this reflected that their ability to regulate host innate immune responses was vital. The human innate immunity imposed a strong selection pressure on SARS-CoV-2 VOCs, whose ancestral strain(s) likely adapted to evade innate immunity in a non-human species.
Omicron S mutations effectively reduced its dependence on transmembrane protease, serine 2 (TMPRSS2) to enter the host and its in vivo tropism in the upper airway. However, compared to Alpha or Delta, Omicron was less effective in suppressing innate immune responses. Omicron lineages, particularly BA.5, after successfully escaping widespread adaptive immune responses, enhanced the capacity to evade innate immunity by expressing higher levels of Orf6 and effectively suppressing interferon (IFN) responses.
Furthermore, the study pinpointed cellular pathways similarly modulated across the VOCs during infection. Thus, combination therapies simultaneously targeting adaptive (e.g., vaccines) and innate immune (e.g., Orf6) responses appear the most suitable as new antivirals. In vivo, therapies targeting host factor(s) essential for viral replication, e.g., eukaryotic translation elongation factor 1A (eEF1A), such as plitidepsin was effective against all VOCs and could even help manage emerging or future SARS-CoV-2 variants.
Conclusions
Integrative computational analyses suggested that VOC evolution eventually converged to suppress interferon-stimulated genes (ISGs), except in Omicron BA.1. Since ISG suppression correlated with innate immunity antagonist protein expression, e.g., Orf6, Orf9b, N, the researchers mapped those to specific mutations.
Overall, the study findings highlighted the plasticity of host-virus interactions and viral protein evolution, suggesting that non-coding point mutations also affected SARS-CoV-2 activity. More importantly, SARS-CoV-2 VOC's convergent evolution overcame human immune barriers.