In 1953, the London Transport Worker's Study highlighted the health benefits of stair climbing by indicating its inverse relationship with coronary artery disease. Despite the attention on stair climbing's cardiovascular impacts, its link to LBP has not been deeply studied. LBP is a widespread issue, with around 8.2% of adults globally and 28% in the United States (US) experiencing it over a 3-month period. While exercise is widely recommended for LBP, its efficacy varies, costing the US an estimated $46 to $200 billion annually. Notably, recent findings suggest LBP may be related to the strength and size of the gluteus maximus (GM). There is an unexplored link between stair climbing, gluteus maximus strength, and LBP prevalence, necessitating further research to develop effective, low-cost interventions.
About the study
The present study, recognized as exempt from the Institutional Review Board Review, utilized a survey developed on the Qualtrics platform. This survey was distributed to physical therapists and members of the American Physical Therapy Association (APTA) Academy of Orthopedic Physical Therapy (AOPT) due to their homogenous educational and socioeconomic backgrounds. Their unified knowledge in areas such as patient medical history and LBP made them ideal respondents. The motivation to design a unique survey tool emerged from the lack of an existing tool covering a broad scope. This survey was inspired by various sources, including the National Health Interview Survey and the International Physical Activity Questionnaire, among others.
For the study's purpose, LBP was defined as pain between the gluteal fold and the 12th rib. The classification of LBP was based on its duration, with chronic LBP identified as pain persisting beyond three months. The survey's validation involved a focus group of physical therapists who provided feedback on various aspects, leading to adjustments in the tool. It was distributed to the APTA AOPT members in September 2022.
Statistical analysis was crucial, and drawing inspiration from Rey-Lopez's data from the Harvard Alumni Study, we determined the required sample sizes. Data, processed using Statistical Package for the Social Sciences (SPSS), underwent various tests like the Kolmogorov-Smirnov test, t-test, and Analysis of Variance (ANOVA) tests to interpret the findings. The statistical significance bar was set at P ≤ 0.05.
Study results
The survey was dispatched to 15,203 individuals via email. Of these, 8,941 opened the email, leading to 363 initiating the survey. Ultimately, 248 final records were used for the analysis after removing incomplete and ineligible records.
Upon analyzing the data, no significant differences emerged in terms of gender, age, weight, height, BMI, years in the physical therapy profession, or work setting between individuals with LBP and those without it. However, despite a distinction surfacing in work status—full-time versus part-time—the correlation between work hours each week and LBP chronicity was found insignificant.
 Greater number of weekly stairs climbed is associated with lower low back pain prevalence among female but not male physical therapists
Greater number of weekly stairs climbed is associated with lower low back pain prevalence among female but not male physical therapists
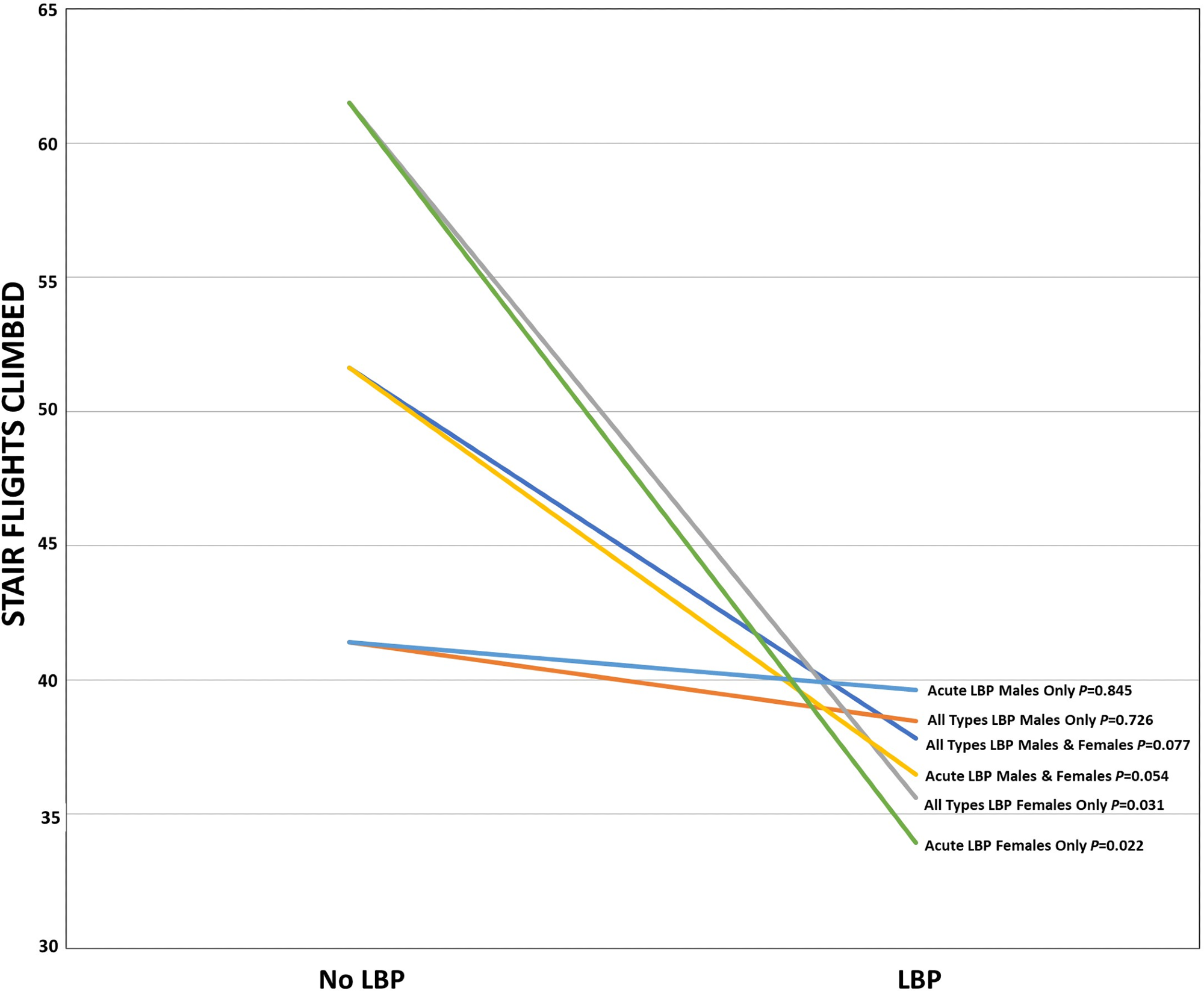
An examination of the average flights of stairs climbed weekly highlighted some notable patterns. While no significant disparity was found between LBP and no LBP (NLBP) respondents when both genders were combined, a difference did surface among female respondents. Female NLBP individuals reported climbing an average of 61.51 flights weekly, whereas their LBP counterparts reported only 35.61 flights.
Moreover, when assessing stair climbing based on LBP duration, the data revealed no significant distinctions across LBP duration groups. However, a clear differentiation appeared among female respondents based on LBP duration. Specifically, those without LBP and those with acute LBP showed significant variations in their stair-climbing habits.
The survey also delved into other physical activities, including both recreational and occupational. Stair climbing stood out as the primary distinction, though weekly resistance training displayed a noticeable difference as well. Individuals without LBP reported a slightly higher intensity in resistance training than those with LBP.
Mental health and sleep patterns were also part of the survey since they are known to have associations with LBP. Results showed no substantial differences between LBP and NLBP participants concerning levels of anxiety, depression, or sleep quality when genders were combined. However, a significant disparity in sleep quality emerged between female LBP and NLBP respondents. This difference persisted even when accounting for age as a potential influencing factor.
Finally, in considering the association between flights of stairs climbed and LBP, the study sought to discern gender-based differences in activity levels when male and female responses were separated. The analysis revealed no notable distinctions between male and female participants concerning any activity's distance, time, or intensity.