In a recent study published in the Proceedings of the National Academy of Sciences (PNAS), researchers analyzed the mortality trends among adults of working age as well as retirement age (above 65 years) in the United States (US) and their relative impact on life expectancy stagnation observed post-2010. They found that increased mortality in the retirement age group, as well as the years of life lost (YLL) and excess deaths in 2019, had a more significant impact on life expectancy stagnation than the increased mortality in the working-age population.
The life expectancy growth in the US has stalled since 2010 despite the advances made in science and healthcare. Previous studies attributed this stagnation to the increased mortality in middle-aged and younger adults, caused mainly by drug overdose, cardiometabolic diseases, and suicide. The present study aimed to analyze, for the first time, the relative contributions to mortality among adults of working age and retirement age in the US.
 Brief Report: The “double jeopardy” of midlife and old age mortality trends in the United States. Image Credit: Hyejin Kang / Shutterstock
Brief Report: The “double jeopardy” of midlife and old age mortality trends in the United States. Image Credit: Hyejin Kang / Shutterstock
About the study
This study used statistical analyses to investigate the impact of mortality trends among working-age and older-age adults on life expectancy stagnation in the US. The term "double jeopardy" is coined to depict the mortality trends in these two age groups.
Annual mortality rates were obtained from the Human Mortality Database. The researchers calculated counterfactual death rates between 2000 and 2019 by extrapolating the average change in all-cause mortality specific to sex and single-year-age-group from 2000–2009 to 2010–2019. They applied these rates to four age groups: above 25 years, 25–49 years, 50–64 years, and above 65 years. Furthermore, the excess deaths and YLL were calculated and summed at each year of age between 5-year age groups.
To comprehensively assess age-specific contributions in situations that differently weight the age groups, the study used three population indicators of mortality: life expectancy, YLL, and excess deaths. The independent effects of mortality rates in working-age and retirement-age adults were mapped to these indicators between 2010 and 2019 and compared to the period 2000 to 2009, when the life expectancy at 25 years of age (e25) increased for women and men by 1.36 years and 1.72 years, respectively.
Results and discussion
As per the findings, e25 increased by 0.41 and 0.17 years for women and men, respectively. Had the trend for mortality in age above 25 years between 2000 and 2009 continued until 2019, e25 would have increased for both men (by 2.1 years) and women (by 1.2 years).
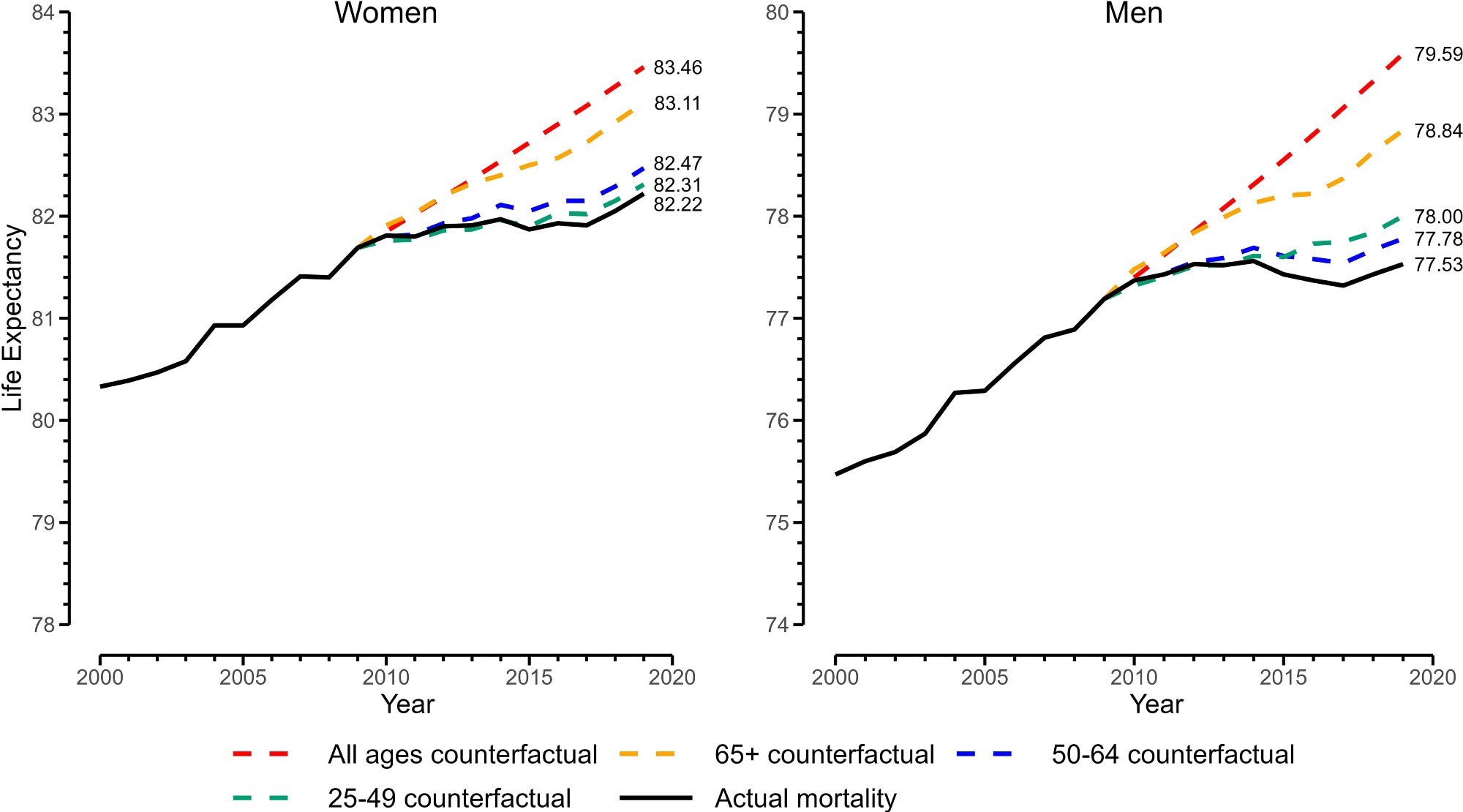 Real and counterfactual life expectancies at age 25, 2000 to 2019. Note: y axis is life expectancy at birth calculated from adding 25 y to e25 (life expectancy at age 25, conditional on surviving to age 25 y).
Real and counterfactual life expectancies at age 25, 2000 to 2019. Note: y axis is life expectancy at birth calculated from adding 25 y to e25 (life expectancy at age 25, conditional on surviving to age 25 y).
To isolate the effect of old age, only the mortality rate of age above 65 years was allowed to continue at its 2000–2009 pace until 2019, while the working-age trends remained at their actual levels. However, instead of retirement age mortality, if the working-age mortality (ages 25–49 years and 50–64 years) were allowed to continue at the 2000–2009 pace until 2019, the e25 would only have increased slightly. These findings thus suggest that although the e25 stagnation is affected by mortality trends at the working age as well as the retirement age, the latter trends have a more significant impact. Furthermore, it was observed that the effect for ages above 65 years was contributed to more by adverse trends in the age group 65–84 than by the age group above 85.
In the excess death analysis, the impact of real and counterfactual death rates was compared on the 2019 population. As per the study, 76% of the 230,000 excess deaths in men and 81% of the 157,000 excess deaths in women occurred at ages above 65 years. Additional analysis shows that the mortality in ages above 65 years accounts for YLL in both women (61%) and men (55%). As per the study, the coronavirus disease 2019 (COVID-19) pandemic further compounded the effect on preexisting life expectancy stagnation post-2019.
The authors discussed various interconnected factors contributing to these mortality trends, such as economic inequality, social isolation, and inadequate healthcare access. The counterfactual death rates presented in this study were comparable to those found in Japan, Switzerland, the United Kingdom, and Italy. Further research is required to better understand the causes of mortality and the contribution of upstream factors to this "double jeopardy."
Conclusion
In conclusion, the findings suggest a greater impact of mortality trends of retirement-age individuals on life expectancy stagnation in the US. The study highlights the urgent need to address the "double jeopardy" of midlife and old age mortality in the US, which may have significant implications for population health and well-being. Comprehensive and coordinated policy interventions aimed at addressing the underlying causes and determinants of these mortality trends could be beneficial for improving health outcomes in the US population.