Long-COVID has become a major public health concern worldwide because of its persistent health and economic implications. According to the World Health Organization (WHO), continuation of COVID-19 symptoms or development of new symptoms three months after the acute infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is referred to as long-COVID.
Approximately 40 million cases of long-COVID have so far been detected worldwide, indicating a high global prevalence. About 72% of patients with self-reported long-COVID experience difficulty in their daily life activities.
In the current study, scientists have estimated the excess primary care costs associated with long-term management of COVID-19 among non-hospitalized patients in the United Kingdom. Moreover, they have explored the relationship between various risk factors and primary care costs.
Study design
The data on non-hospitalized COVID-19 patients obtained from a large primary care UK database was analyzed in the study. Long-COVID was defined as having persistent symptoms 12 weeks after acute SARS-CoV-2 infection.
Two groups of patients were selected from the database. The exposed group included adult patients with laboratory-confirmed COVID-19 who had not been hospitalized 14 days before or 42 days after the acute infection. The unexposed group included adult individuals without any history of suspected or confirmed COVID-19.
The additional cost related to long-COVID primary care consultation was estimated both at the individual level and the UK national level. Multivariable regression analysis was conducted to estimate the association between risk factors and primary care consultation costs beyond 12 weeks from acute COVID-19.
Important observations
A total of 472,173 COVID patients and 472,173 unexposed individuals were included in the study analysis. Among COVID patients, about 0.8% and 6.4% had diagnosed long-COVID and symptomatic long-COVID, respectively.
The estimation of the number of consultations revealed a 22.7% higher consultation rate in the exposed group than in the unexposed group. Among patients with diagnosed long-COVID and symptomatic long-COVID, the consultation rates were 3-times and 6-times higher, respectively, compared to that among patients with previous COVID-19 but no long-COVID related symptoms.
The annual incremental cost of long-COVID primary care consultations was estimated to be £2.44 at the individual level and £23,382,452 at the national level. The incremental costs in the diagnosed and symptomatic long-COVID groups were £30.52 and £57.56 per patient, respectively.
For each study group, more than 85% of the total costs were related to general physician (GP) consultations. The average cost per patient was higher in all COVID-19-related groups compared to that in the unexposed group. The highest expense was observed in the symptomatic long-COVID group across each type of healthcare professional.
More than 60% of the total costs for each study group were associated with telephonic consultations. The incremental costs associated with home visits were higher in the exposed group compared to those in the unexposed group. The most significant contributor to the total cost in the unexposed group was in-person consultations.
Association between risk factors and primary care consultation costs
The risk factor analysis revealed that the primary care consultation costs were 43% and 44% higher among patients with diagnosed long-COVID and symptomatic long-COVID, respectively, compared to that among exposed patients without a long-COVID diagnosis or related symptoms.
Other risk factors that increased the cost of primary care consultation were older age, female gender, obesity, comorbidities, frequency of previous consultations, and White ethnic group.
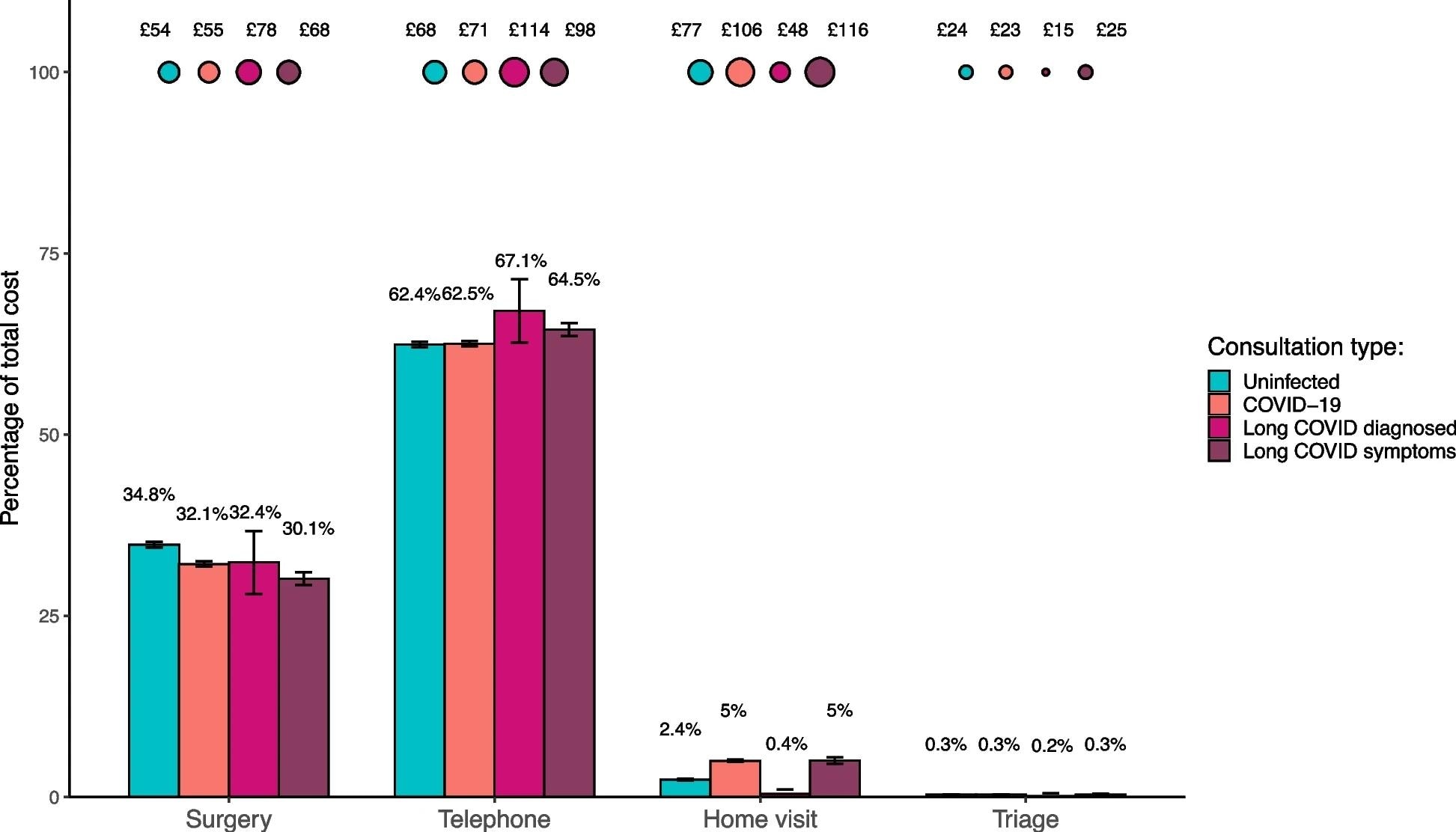 Bubble plot to show the average cost of each consultation type per patient (who had a consultation) between 15th April 2020 and 15th April 2021. Bar chart to show the percentage makeup of each group's total costs by consultation type
Bubble plot to show the average cost of each consultation type per patient (who had a consultation) between 15th April 2020 and 15th April 2021. Bar chart to show the percentage makeup of each group's total costs by consultation type
Study significance
The study finds that the cost of primary care consultation associated with long-COVID management is substantially high among non-hospitalized patients. Specifically, the costs are significantly higher among patients with diagnosed long-COVID or related symptoms, older patients, female patients, obese patients, and those with comorbidities.
The cost estimates provided by the study could be helpful for future cost analyses and economic evaluations on long-COVID, which is crucial for the preparedness for future pandemics.