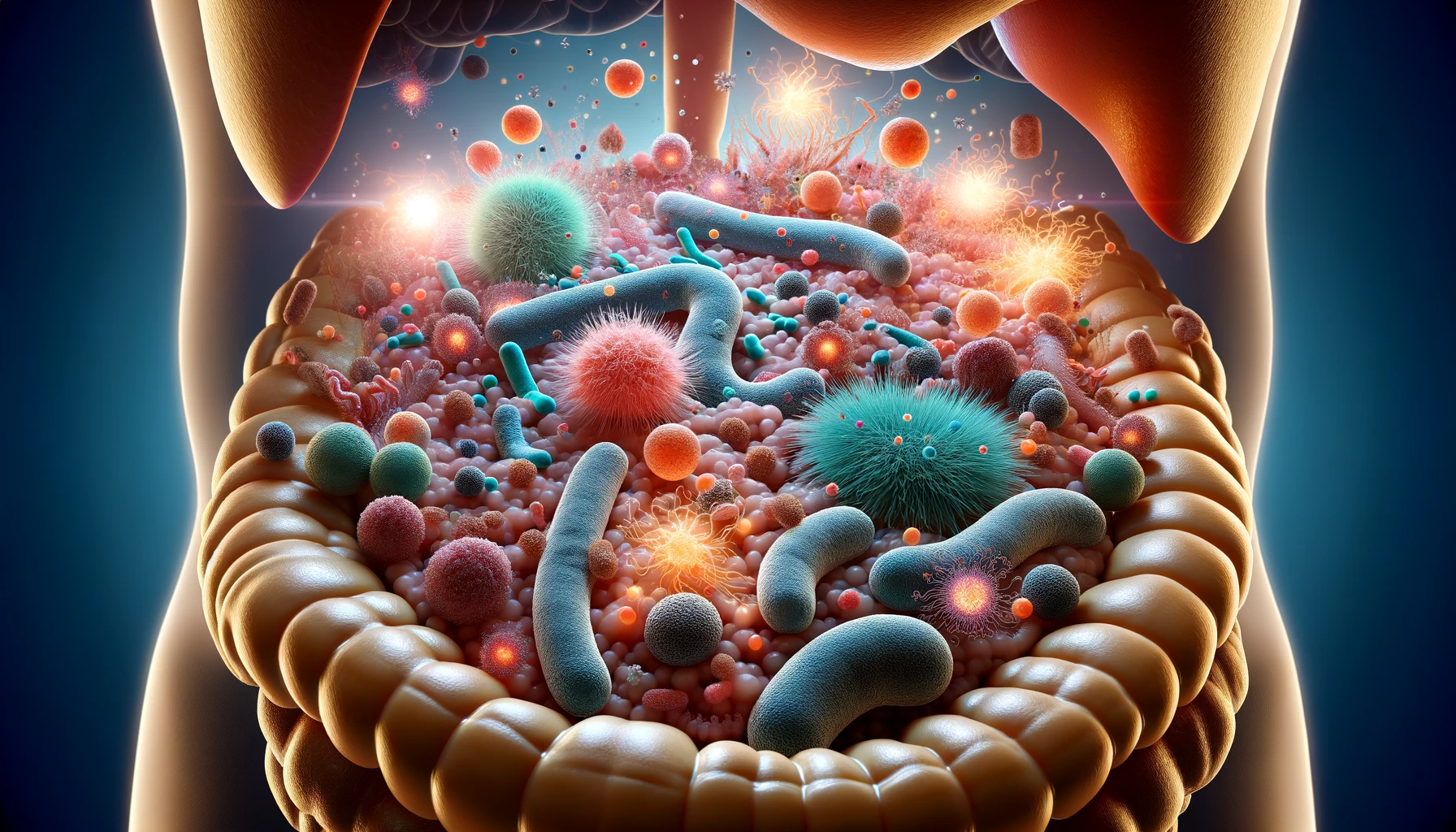
SAD, a mental condition defined by anxiety or acute dread in social situations, commonly begins in childhood and results in permanent functional impairment and impaired life quality. Current therapies are insufficient and ineffectual, and innovative models are required to comprehend the underlying biology and therapy targets. According to recent research, the gut microbiome is involved in behavioral and brain-related activities connected to social interactions.
 Study: Social anxiety disorder-associated gut microbiota increases social fear
Study: Social anxiety disorder-associated gut microbiota increases social fear
About the study
In the present study, researchers investigated whether gut microbes are causally involved in promoting host social fear behavior.
The team investigated the microbiota of individuals with severe anxiety disorder (SAD) and healthy controls (HC). They characterized the gut microbial composition using 16S ribosomal ribonucleic acid (rRNA) sequencing on microbial deoxyribonucleic acid (DNA) isolated from stool samples provided by the participants. They administered adult C57Bl/6J mice with a fecal microbiota transplant (FMT) from donors. The team tested the mice for sociability, social fear, cognition, stress-coping behaviors, gastrointestinal evacuation, and motility. The researchers used social fear conditioning and extinction learning the following day to evaluate social behavior by measuring interaction time after recurrent exposures to new social and non-social stimuli.
The team measured murine plasma corticosterone levels pre- and post-forced swim assessments using corticosterone enzyme-linked immunosorbent assays (ELISA). After euthanasia, ileal tissues were explanted and treated with concanavalin A (ConA), lipopolysaccharide (LPS), clusters of differentiation 3 and 28 (CD3/CD28) clusters, or a buffer vehicle to compare gut immune activity in reaction to archetypal antigens. In addition, the researchers harvested blood and mesenteric-type lymph nodes (MLNs) to asses immunological cell populations by flow cytometry.
To discern the impact on central immunity, the team measured neuroinflammatory- and blood-brain barrier-related gene expression in the bed nucleus of the stria terminalis (BNST), medial amygdala (MeA), and medial prefrontal cortex (MePFC). In addition, they measured oxytocin in the paraventricular nucleus (PVN), supraoptic nucleus (SON), and the BNST by immunohistochemistry.
The researchers placed mice on an antimicrobial cocktail comprising ampicillin, vancomycin, and imipenem. They prepared SAD and control group fecal inocula for fecal microbial transplantation four hours post-production. Animals received fecal microbial transplants through oral gavage (100.0 μL) every day for three days and two booster fecal microbiota transplants weekly for the rest of the assessment period (10 FMTs total).
Results
The SAD murine microbiota had a differential composition compared to healthy controls. SAD significantly altered beta diversity. At study completion, three species of bacteria showed lowered abundances in the SAD study group, i.e., Bacteroides cellulosiyticus, Phocaeicola massiliensi, and Bacteroides nordii. No group-specific variations were found in the Simpson, Chao1, and Shannon alpha diversity metrics, although each metric showed reduced values.
Following antibiotic bacterial depletion, fecal microbiota transplants from the SAD and control group donors resulted in differential microbial recolonization and engrafting. The mice that received the SAD microbiota had a specific heightened susceptibility to social anxiety, a model of SAD, coupled with changes in central and peripheral immune function and oxytocin expression in the BNST.
Over the six social stimulus trials, considerable reductions in social engagement were observed, demonstrating that SAD microbes might enhance susceptibility to social apprehension cues. However, SAD FMT did not affect general sociability, social novelty choice, stress-coping behaviors, or gastrointestinal transit, showing that sensitivity to social fear was transferred specifically. The SAD microbiota reduced immune function and stress, significantly reducing corticosterone concentrations by SAD fecal microbial transplantation. The SAD microbes also showed a reduced interleukin 17A (IL-17A) response to LPS and ConA stimulation.
After SAD FMT, F4/80+-type macrophages in MLNs decreased significantly, while helper T cells increased. SAD microbial transfer reduces circulating stress hormones and peripheral immunity. SAD FMT led to a decrease in arginine-1 expression in three regions, reducing chemokine C-X-C ligand 15 (CXCL-15), interleukin 10 (IL-10), and tumor necrosis factor-alpha (TNF-α). The findings indicated that SAD FMT altered neuroinflammatory markers and impaired blood-brain barrier (BBB) function, highlighting the microbiota's immunomodulatory potential. The findings linked lowered neuronal oxytocin levels within the stria terminalis and oxytocin-associated gene expression in the prefrontal cortex and medial amygdala to increased social anxiety behavior.
The study findings showed that the microbiome plays a crucial role in social fear responses and could be a potential therapeutic target for SAD. Human patients with SAD showed similar beta-diversity microbiota composition alterations to recipient mice. Phocaeicola massiliensis, Bacteroides nordii, and Bacteroides cellulosilyticus counts were lower in the SAD group than in healthy controls. Following social fear conditioning, SAD group social interaction decreased significantly, indicating that a SAD microbial transfer can intensify the social fear response.