Researchers uncover how emotional eating and body dissatisfaction silently shape our weight and well-being, offering critical insight for better obesity and mental health strategies.
 Study: Pathways linking BMI trajectories and mental health in an adult population-based cohort: role of emotional eating and body dissatisfaction. Image Credit: Nicoleta Ionescu / Shutterstock
Study: Pathways linking BMI trajectories and mental health in an adult population-based cohort: role of emotional eating and body dissatisfaction. Image Credit: Nicoleta Ionescu / Shutterstock
In a recent study in the International Journal of Obesity, researchers investigated the role of emotional eating and body dissatisfaction in weight change trajectories and mental health. The study included 7,388 adult participants who had been followed over four years and employed mixed effects and regression models for data analyses.
Study findings revealed that both emotional eating and body dissatisfaction independently mediate suboptimal outcomes. Emotional eating partly mediated the association between baseline anxiety and depressive symptoms and increasing body mass index (BMI), while body dissatisfaction and self-rated health partly mediated the association between increasing BMI and reduced overall quality of life (QoL).
Interestingly, BMI trajectories were not associated with anxiety and depressive symptoms at follow-up after accounting for baseline mental health, although they were linked to body dissatisfaction and lower QoL.
The association between emotional eating and BMI trajectories was stronger among women and individuals with low physical activity levels.
These findings suggest the presence of a potential bidirectional relationship, where emotional eating and body dissatisfaction contribute to BMI increases, which in turn further influence these mediators and negatively affect quality of life.
Background
Overweight and obesity present significant public health concerns. While the World Health Organization (WHO) projects that 20% of the global population will have obesity by 2025, current prevalence estimates suggest that over 1 billion people live with excessive body mass index (BMI). These conditions are frequently associated with chronic diseases, including type 2 diabetes (T2D), cardiovascular diseases (CVDs), and certain cancers. These associations were referenced in the context of public health but were not directly investigated in the study.
Mental health concerns present another substantial public health concern, with depression and anxiety afflicting an estimated 970 million people worldwide. Previous research employing extensive population-wide datasets and long follow-up periods has established the positive bidirectional relationship between overweight and adverse mental health outcomes. More recent research has further validated the roles of biological mediators (inflammation and gut microbiota) in promoting these outcomes.
Unfortunately, these studies have failed to investigate the effects of psychosocial and behavioral mediators, such as emotional eating and body dissatisfaction, on altering BMI and mental health outcomes.
About the study
The present study aims to address these gaps in the literature by utilizing a large, long-term follow-up adult cohort to provide insights into:
- The psychosocial and behavioral predictors of BMI trajectories,
- The impacts of these BMI trajectories on mental health, and
- How emotional eating and body dissatisfaction influence BMI and mental health outcomes.
Study data were obtained from the Specchio cohort, a digital follow-up study of Geneva (Switzerland) COVID-19 serosurvey participants. The study was launched in December 2020 and included 13,260 participants who completed an inclusion questionnaire at baseline. Participants who included their heights and weights in the baseline questionnaire were included in the present study.
BMI measurements were calculated from participant-provided height and weight data obtained at baseline and again in 2022, 2023, and 2024. WHO guidelines were referenced to classify participants into: 1. underweight (BMI < 18.5 kg/m²), 2. healthy (BMI 18.5–24.9 kg/m²), 3. overweight (BMI 25.0–29.9 kg/m²), 4. obesity (BMI 30–39.9 kg/m²), and 5. severe obesity (BMI ≥ 40 kg/m²).
Custom prevalidated questionnaires were used to record participants’ behavioral factors (physical activity, diet, alcohol consumption, sleep patterns, leisure time, anti-depressant medication, and emotional eating) and psychosocial factors (social and psychological resources and risks). The questionnaire also incorporated the WHO’s well-being index to measure participants’ mental and general health outcomes.
The Oslo Social Support Scale was used to translate perceived resources and risks into analyzable data. Additionally, the Brief Rosenberg Self-Esteem Scale was used to evaluate participants’ perceptions of self-esteem. Statistical analyses included mixed effects models for estimating BMI trajectories and regression models for both sets of association determination (behavioral/psychosocial factors and BMI trajectories, and BMI trajectories and mental health). Models were adjusted for participants’ age, sex, education, and pre-existing health conditions.
Structural equation modeling was used to test mediation pathways and assess indirect effects.
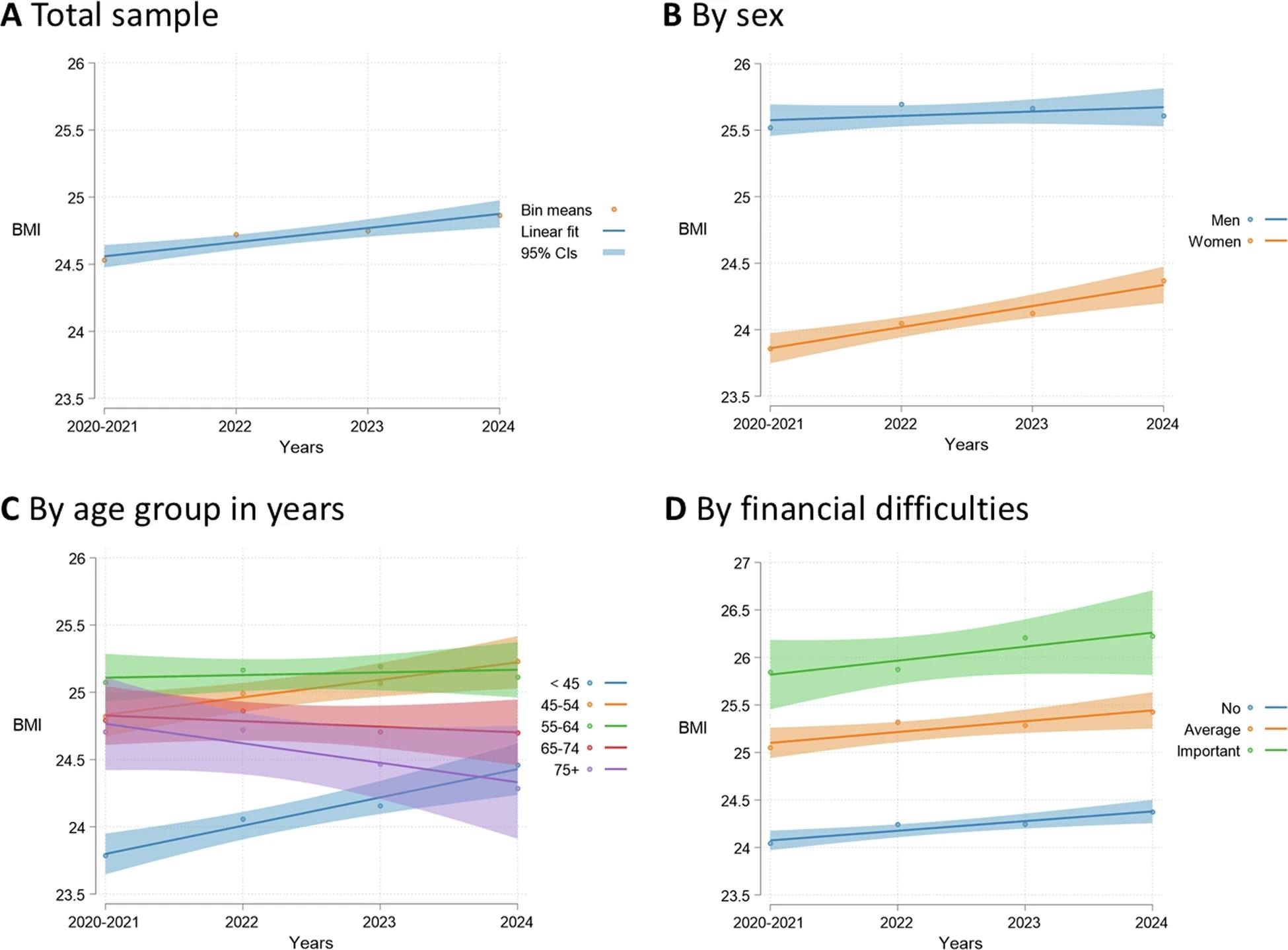 Trends in BMI over time for the total study sample, and by sex, age group, and financial difficulties (N = 7388).
Trends in BMI over time for the total study sample, and by sex, age group, and financial difficulties (N = 7388).
Study findings
Of the 13,260 participants in the Specchio cohort, 7,388 (59% female) met the inclusion criteria and were included in downstream analyses. The average age of included participants was 51 years, with a mean estimated BMI of 24.5 kg/m².
Study findings revealed that participants’ BMI slightly increased (0.4 kg/m²) throughout the study (4 years) at the whole sample cohort scale.
“Most of the sample (86%) had the same BMI classification at follow-up as at baseline. 8% of the sample had an upward BMI classification trajectory, transitioning from healthy weight to overweight (5%), from overweight to obesity, or from obesity to severe obesity (3%). 5% had a downward BMI classification trajectory. By 2024, 43% of the sample had overweight or obesity.”
Mixed effects models revealed that the leading psychosocial and behavioral causes for changing BMI trajectories included a reduction in physical activity levels, financial difficulties, reduced sleep, increased screen time, depression/anxiety, and emotional eating.
Increased BMI was, in turn, associated with increases in participants’ body dissatisfaction and lower overall quality of life (QoL). These findings remained robust even after accounting for mental health conditions. Notably, BMI increases were not significantly associated with anxiety or depressive symptoms at follow-up after adjusting for baseline scores.
Structural equation modeling revealed that emotional eating partly mediated the effect of baseline anxiety and depressive symptoms on increasing BMI, as well as the association between financial hardship and BMI trajectories. Body dissatisfaction and poorer self-rated health partly mediated the relationship between increasing BMI and reduced QoL.
The authors noted that these mediation effects were statistically significant but modest in size.
The relationship between emotional eating and BMI was found to be stronger among women and those reporting low levels of physical activity, suggesting possible targets for tailored intervention.
Conclusions
The present study highlights the impacts of emotional eating and body dissatisfaction in contributing to rising BMI and adverse mental health outcomes, which in turn may promote further emotional eating and dissatisfaction. While the data support directional mediation pathways, the study does not establish a formal feedback loop.
Importantly, the authors noted several limitations, including the observational design, reliance on self-reported BMI and emotional eating data, and the lack of clinical measures for mental health. These factors may limit the ability to draw causal inferences.
These findings are essential in developing prevention and intervention strategies against these public health concerns (obesity and mental health conditions).
“Our study highlights emotional eating and body dissatisfaction as important factors associated with BMI trajectories and mental health, and to be considered in weight management and mental health promotion strategies.”
Journal reference:
- Schrempft, S., Jiménez-Sánchez, C., Baysson, H. et al. Pathways linking BMI trajectories and mental health in an adult population-based cohort: role of emotional eating and body dissatisfaction. Int J Obes (2025). DOI: 10.1038/s41366-025-01772-y. https://www.nature.com/articles/s41366-025-01772-y