The body's immune response to Epstein-Barr virus (EBV) may play a role in causing damage in people with multiple sclerosis, according to a new study led by UTHealth Houston.
EBV infection has long been associated with multiple sclerosis, but how the infection might contribute to multiple sclerosis has not been clear. More than 95% of people have been infected with this prevalent virus; however, it typically remains in its latent stage and doesn't cause any issues. In some cases, though, the T-cells specific for the EBV infection may cause problems.
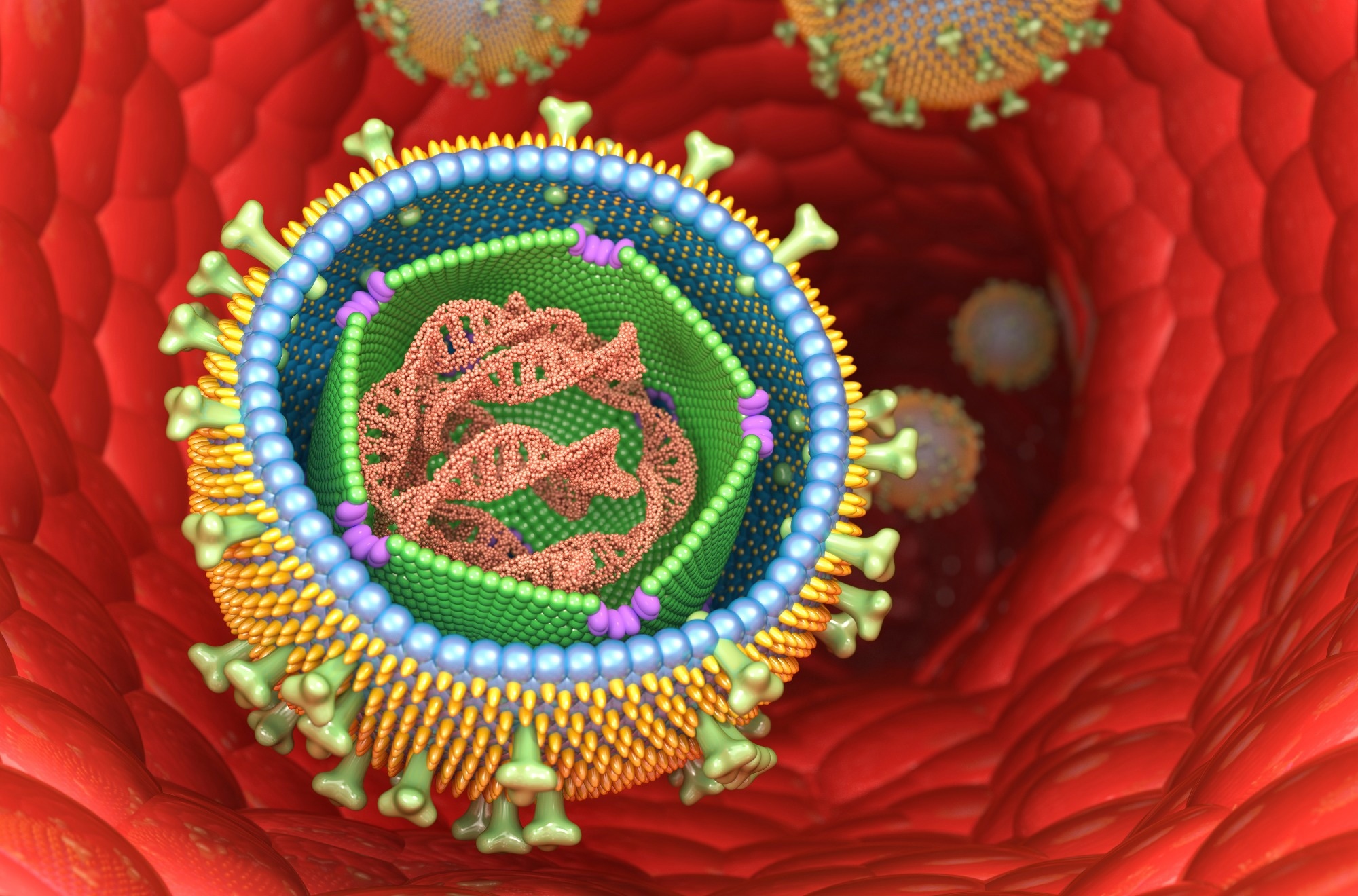 Study: Expanded T lymphocytes in the cerebrospinal fluid of multiple sclerosis patients are specific for Epstein-Barr-virus-infected B cells. Image Credit: 3d_man / Shutterstock
Study: Expanded T lymphocytes in the cerebrospinal fluid of multiple sclerosis patients are specific for Epstein-Barr-virus-infected B cells. Image Credit: 3d_man / Shutterstock
Now, research led by first author Assaf Gottlieb, PhD, assistant professor with the Center for Precision Health at McWilliams School of Biomedical Informatics at UTHealth Houston, and senior author J. William Lindsey, MD, professor in the Department of Neurology with McGovern Medical School at UTHealth Houston, demonstrates that T-cells specific for EBV-infected cells are present in high numbers in the cerebrospinal fluid of people with multiple sclerosis at its earliest stages.
The study was published in the journal Proceedings of the National Academy of Sciences.
The researchers obtained blood and cerebrospinal fluid samples from eight patients in the process of multiple sclerosis diagnosis. They stimulated cells from the patient's own blood with multiple different stimuli, including EBV-infected lymphoblastoid cell lines (LCLs) from the same person, cell-free EBV, varicella zoster virus (chicken pox), influenza virus, and candida; they then used RNA sequencing for T-cell receptors to determine which of the stimuli the cerebrospinal fluid T-cells were responding to.
"We saw a clear signal of enrichment of T-cells specific for LCL in the cerebrospinal fluid from the multiple sclerosis patients," said Gottlieb, who is also a faculty member with The University of Texas MD Anderson Cancer Center UTHealth Houston Graduate School of Biomedical Sciences. "This pattern was very different from what we observed in other neurologic diseases, suggesting it is unique to multiple sclerosis."
On average, 13% of the T-cells in the cerebrospinal fluid of people with the first symptoms of multiple sclerosis are specific for autologous B lymphocytes infected with EBV, demonstrating a clear link between EBV and multiple sclerosis.
In the most expanded cerebrospinal fluid clones, which are highly likely to play a role in multiple sclerosis pathogenesis, the abundance of LCL-specific T-lymphocytes is even higher, at 47%.
T-cells for the three other common infections did not show a similar abundance in the cerebrospinal fluid.
"This work demonstrates that T-cells specific for LCL are present in the cerebrospinal fluid at the earliest stages of the disease," said Lindsey, the Opal C. Rankin Professor in Neurology at the medical school. "This strongly suggests that these T-cells are either causing the disease or contributing to it in some way. We have experiments in progress to define what these cells may be doing."
EBV is a member of the herpes virus family that spreads most commonly through bodily fluids, especially saliva, and can cause infectious mononucleosis, among other illnesses.
Multiple sclerosis is a chronic disease of the central nervous system that affects over 1.8 million people globally, according to the World Health Organization. Symptoms vary widely between patients, but some people with severe multiple sclerosis may lose the ability to walk independently. There is no cure for the disease.
Co-authors included H. Phuong T. Pham, Ph.D., formerly with the Department of Neurology at McGovern Medical School and now with The University of Texas at Dallas, and Jerome G. Saltarrelli, Ph.D., with the medical school's Department of Surgery. The research was funded by the Opal C. Rankin Professorship in Neurology and by a pilot grant from UTHealth Houston.
Source:
Journal reference: