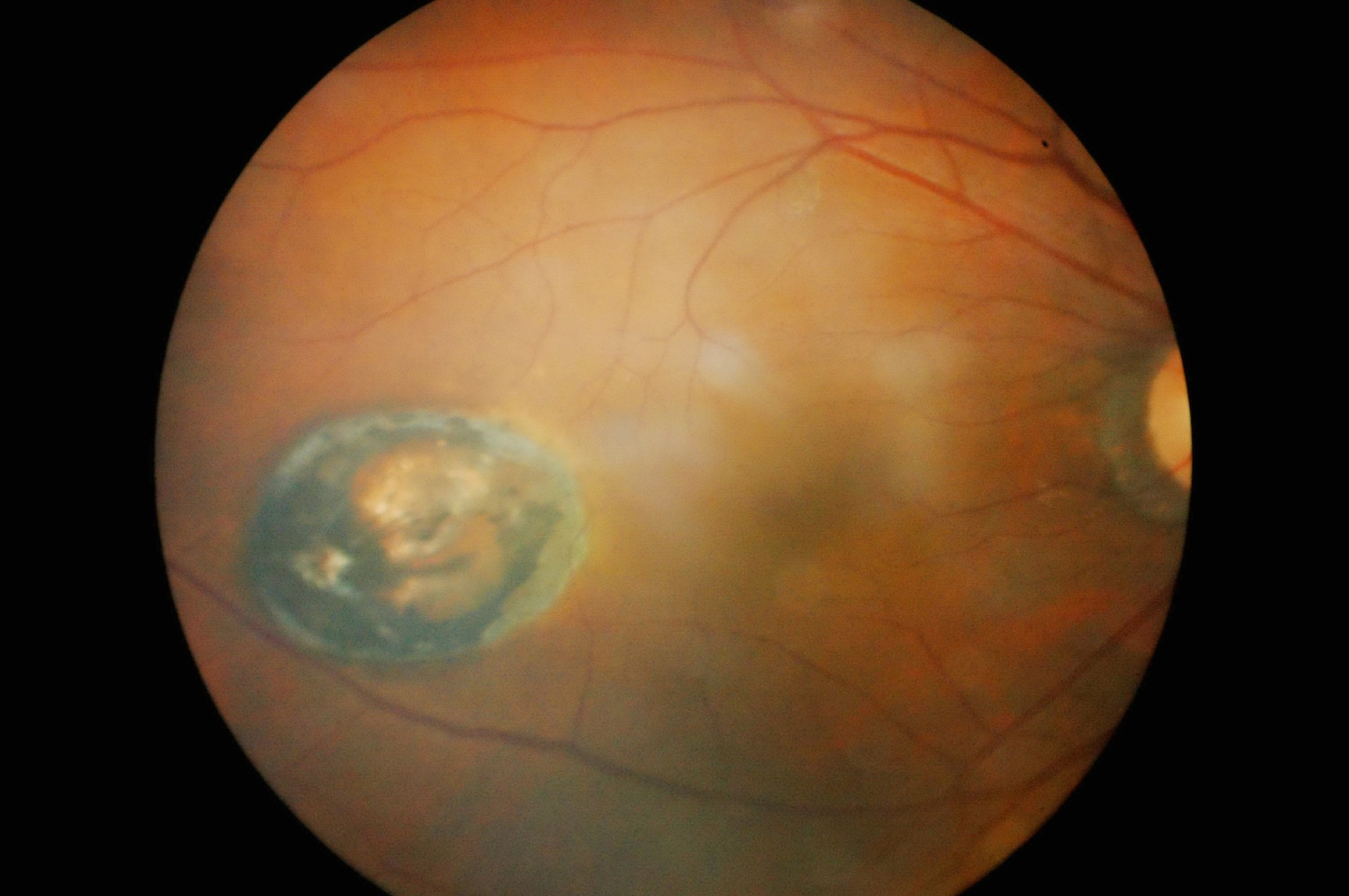
The retina is vascularized to support the higher energetic demand for vision. As such, the neural retina and associated blood vessels are susceptible to metabolic perturbations, like in diabetic retinopathy (DR). Blood-retina barrier breakdown at various stages of DR leads to DME, wherein extravasation of plasma and proteins into intra- and sub-retinal spaces causes swelling and vision loss.
Current standard care for DME involves anti-vascular endothelial growth factor (VEGF) agents, which reduce macular edema and improve visual acuity. However, therapeutic response remains sub-optimal in most patients, with its effectiveness waning over time. Besides, while corticosteroids can effectively reduce edema, they can increase intraocular pressure. Exploring alternative safer, long-lasting, disease-modifying DME treatments can benefit patients.
 Study: Therapeutic targeting of cellular senescence in diabetic macular edema: preclinical and phase 1 trial results. Image Credit: Anukool Manoton / Shutterstock
Study: Therapeutic targeting of cellular senescence in diabetic macular edema: preclinical and phase 1 trial results. Image Credit: Anukool Manoton / Shutterstock
The study and findings
In the present study, researchers investigated how senescent cells contribute to DME. First, they estimated the levels of prototypical senescence-associated secretory phenotype (SASP) factors in DME patients’ vitreous. This revealed increases in interleukin (IL)-6, IL-8, and plasminogen activator inhibitor 1 (PAI1) levels in DME patients relative to controls with non-vascular pathology.
Further, the expression of p16INK4A, a cell cycle regulator associated with senescence, in postmortem retinal sagittal sections of DME patients compared to age- and sex-matched non-diabetic control retinas. Increased p16INK4A expression was observed in the inner retina, choroidal layers, and Bruch’s membrane in retinas with DME. p16INK4A expression was confined to regions of suspected disease activity.
Next, the researchers examined bulk RNA sequencing (RNA-seq) datasets of retinas from mice and rats with streptozotocin (STZ)-induced diabetes. Genes for cellular senescence and the SASP were positively correlated in STZ-treated animals compared to controls. For increased resolution, they assessed single-cell RNA-seq (scRNA-seq) datasets from mice with STZ-induced diabetes.
Cone photoreceptors, endothelial cells (ECs), and Muller glia were the most transcriptionally perturbed populations compared to non-diabetic controls. Sub-clustering of ECs disclosed three distinct sub-clusters (EC1 – EC3). EC2 was predominant in diabetic retinas and was enriched for genes linked to vascular complications in diabetes and those involved in regulating cellular senescence in ECs and other cell types.
Further experiments suggested that senescent ECs in the retina impaired barrier function. Next, whether hyperglycemia could trigger senescent phenotypes in DME was evaluated. Human retinal microvascular ECs (HRMECs) were exposed to a medium with high D-glucose (HG) or isosmotic control enantiomer (CTR). After five weeks of HG exposure, global cellular proliferation decreased by 25%, and cells with senescence-associated markers increased three-fold compared to CTR.
Anti-apoptotic proteins such as B-cell lymphoma 2 (BCL2) and BCL-xL were induced in HG-treated HRMECs. Further, the researchers tested whether targeting BCL-xL could improve barrier function in diabetic retinas. A small-molecule inhibitor, UBX1967, was administered intravitreally to diabetic mice eight and nine weeks after STZ treatment. This significantly reduced protein levels of BCL-xL and PAI1 at 10 weeks of diabetes.
Retinal BCL2 levels were unaltered, while transcript levels of inflammatory SASP factors were significantly reduced. Notably, UBX1967 treatment reduced retinal vascular permeability by 40% to 50%. In addition, whole-field scotopic electroretinography showed that UBX1967 treatment improved retinal function. The researchers developed UBX1325, a phosphate pro-drug with senolytic properties, as a therapeutic candidate.
BCL-xL target engagement was confirmed for UBX0601 (active molecule of UBX1325) in senescent HRMECs. The researchers noted that apoptosis initiation through BCL-xL inhibition required senescent cells to be present. Apoptosis with BCL-xL inhibition did not occur in healthy retina. UBX1325 also decreased retinal vascular permeability (40% – 50%) in the STZ model compared to vehicle-treated controls.
Next, the team performed a phase 1 safety and tolerability trial of UBX1325 in patients with advanced DME or neovascular age-related macular degeneration for whom anti-VEGF therapy was no longer beneficial. Intravitreal UBX1325 injection was well tolerated with no reports of inflammation. However, a few treatment-emergent adverse events (TEAEs) were observed that were deemed unrelated to UBX1325.
TEAEs were more likely observed in patients receiving higher doses, which were considered due to their underlying disease. Initial safety assessment suggested that UBX1325 could be advanced into later-stage clinical studies. Plasma levels of UBX1325 and UBX0601 were below the lower quantification limit. Among DME patients, a single injection improved visual acuity. Higher UBX1325 doses reduced central subfield thickness.
Conclusions
Together, the findings illustrate that therapeutic clearance of senescent cells could result in long-term improvements in visual function in DME patients. Intravitreal administration of BCL-xL inhibitor eliminated senescent ECs, resulting in lower local inflammation and improved barrier function, ultimately augmenting visual function. Efficacy data suggested that vision improvements persist for at least six months.
Journal reference:
- Crespo-Garcia S, Fournier F, Diaz-Marin R, et al. Therapeutic targeting of cellular senescence in diabetic macular edema: preclinical and phase 1 trial results. Nat Med, 2024, DOI: 10.1038/s41591-024-02802-4, https://www.nature.com/articles/s41591-024-02802-4