Coronavirus disease 2019 (COVID-19), caused by SARS-CoV-2, presents influenza-like manifestations, including mild-to-severe pneumonia, acute respiratory distress syndrome, multiorgan failure, and fatal lung injury. Further, the etiology and pathogenesis of COVID-19 are not entirely understood and targeted therapies remain inadequate.
The viral spike protein binds to the host receptor, angiotensin-converting enzyme 2 (ACE2), for cellular entry. Although SARS-CoV-2 preferentially infects cells in the respiratory tract, the virus has been detected in virtually all organs. Studies have revealed the presence of SARS-CoV-2 RNA in diverse cells lacking ACE2, suggesting that other receptors or co-receptors may mediate viral entry.
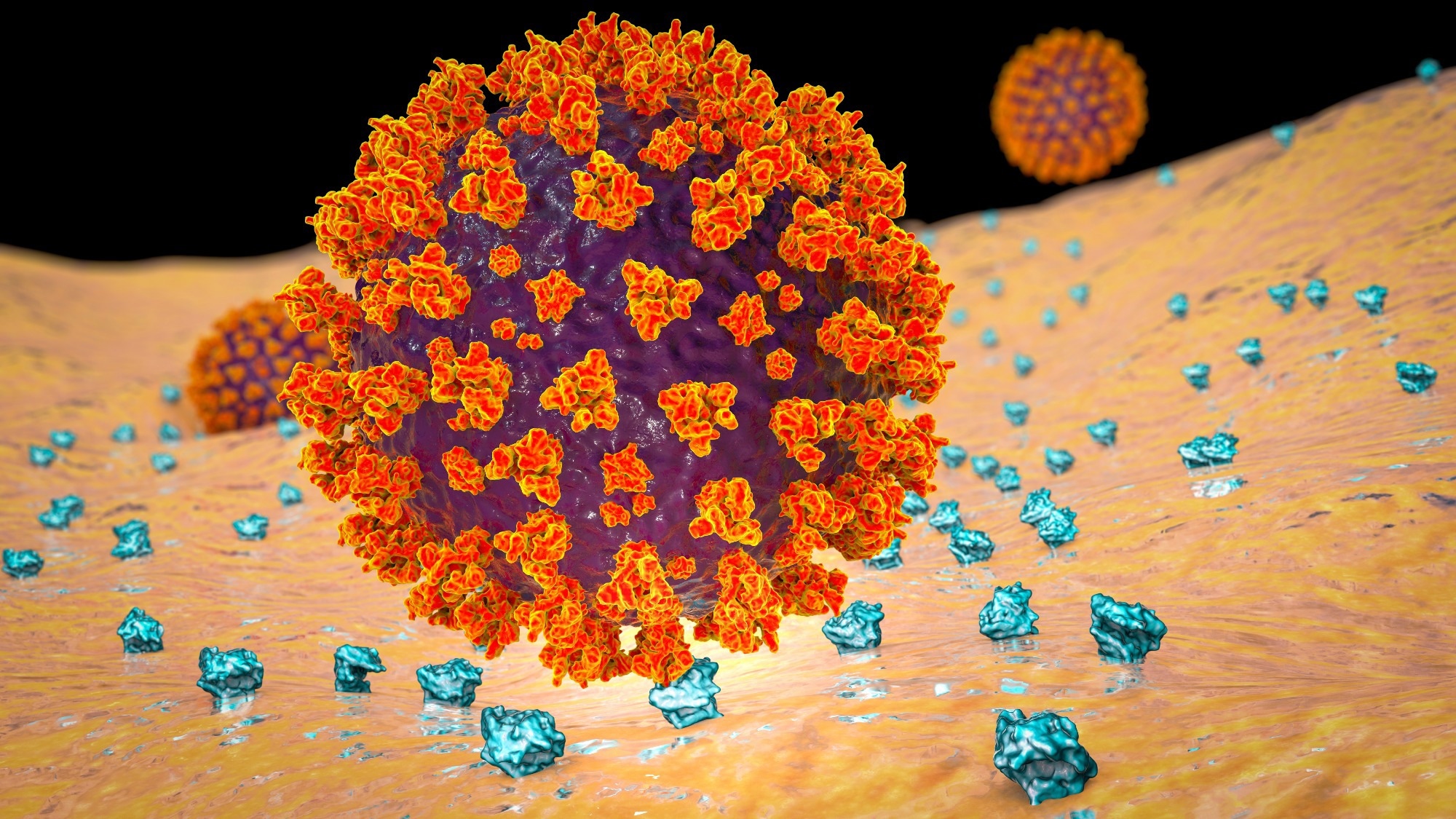 Study: Human transferrin receptor can mediate SARS-CoV-2 infection. Image Credit: Kateryna Kon / Shutterstock
Study: Human transferrin receptor can mediate SARS-CoV-2 infection. Image Credit: Kateryna Kon / Shutterstock
The study and findings
In the present study, researchers identified TfR as an alternative receptor mediating the cellular entry of SARS-CoV-2. First, they used co-immunoprecipitation (Co-IP) to identify host proteins interacting with the viral spike in Calu-3 cells. This revealed 293 proteins, including 42 transmembrane proteins; two proteins were associated with entry (ACE2 and TfR). Next, the team evaluated TfR expression in the respiratory tract and liver in mice.
TfR expression, both transcript and protein levels, was substantially higher in the lungs and trachea than in other tissues. Using immunohistochemical analysis, the researchers investigated the effects of SARS-CoV-2 on TfR expression in the lungs of humanized ACE2 (hACE2) mice and monkeys. This revealed a 1.5- and 1.8-fold increase in TfR expression in mice and monkeys, respectively.
In addition, surface plasmon resonance revealed direct interactions between the viral spike and human TfR. Notably, the spike protein lacked interactions with Syrian hamster or mouse TfR. Docking analysis predicted two peptide sequences (QK8: QDSNWASK and SL8 SKVEKLTL) in TfR to be involved at the interface of TfR-spike interactions.
Mutagenesis and Co-IP revealed that the A529 residue in TfR was essential for interactions with the spike. Further analysis indicated that physiological interactions between spike and TfR occurred at the cellular surface and during endocytosis. This was confirmed by electron microscopy using SARS-CoV-2 pseudoviral spike and HEK293/hACE2 and BHK-21/TfR cells.
Next, the team evaluated the effects of soluble TfR, anti-TfR antibody, and SL8 and QK8 peptides on SARS-CoV-2 infection using reverse-transcription polymerase chain reaction (RT-PCR) and plaque assays. Results showed their inhibitory effects on SARS-CoV-2 in Vero E6 and Calu-3 cells. Cytotoxicity was not observed even at 1,000 nM.
Confocal microscopy revealed that TfR was widespread on the surface of Calu-3 and Vero E6 cells, with the colocalization of TfR and SARS-CoV-2 at the surface and during endocytosis. Notably, treatment with the anti-TfR antibody inhibited the colocalization. Further, electron microscopy showed that viral particles were present in the cytosol and clathrin-coated pits in Vero E6 cells; likewise, treatment with anti-TfR antibody inhibited viral internalization.
Next, ACE2 was knocked out (KO) from Calu-3 and Vero E6 cells and the cells were infected with SARS-CoV-2. This inhibited infection by 40% to 50%, suggesting that ACE2 might not be the only receptor mediating infection. In addition, TfR knockdown (KD) inhibited infection by 30%, whereas its overexpression (OE) promoted infection. TfR KO was not performed as it is lethal. TfR OE or KD did not impact ACE2 expression.
Further, the team transfected C57 mice with adenovirus vector (Ad5) expressing hACE2 or humanized TfR (hTfR) and infected them with SARS-CoV-2. Viral load in the lungs in Ad5-hTfR and Ad5-hACE2 mice was significantly higher than in Ad5-empty mice. Finally, the researchers evaluated the effects of the anti-TfR antibody on infection in rhesus macaques. Anti-TfR antibody inhibited viral replication and reduced pneumonia.
Viral load in the respiratory epithelium was also significantly lower between 3- and 7 days post-infection (dpi) compared to controls. Radiographs taken at 0 and 5 dpi revealed significantly less severe pulmonary infiltration in antibody-treated macaques relative to controls. Antibody-treated animals had no significant pulmonary lesions, while controls showed lung lesions of varying degrees.
Conclusions
Taken together, the study described the human TfR as a receptor for SARS-CoV-2. TfR can directly bind to the viral spike at an affinity comparable to that of ACE2. Notably, mouse TfR and the viral spike lacked interactions. Soluble TfR, SL8, and QK8 peptides and anti-TfR antibodies can inhibit infection. The team also illustrated the antiviral effects of the anti-TfR antibody in rhesus macaques. Overall, TfR could serve as an alternative infection pathway, facilitating viral entry through endocytosis.