In a recent review published in the journal Nature Reviews Microbiology, researchers discussed the epidemiology, treatment options, and emerging antimicrobial resistance (AMR) in sexually transmitted bacterial infections caused by Neisseria gonorrhoeae (the causative agent of gonorrhea), Mycoplasma genitalium, Chlamydia trachomatis, and Treponema pallidum (the causative agent of syphilis).
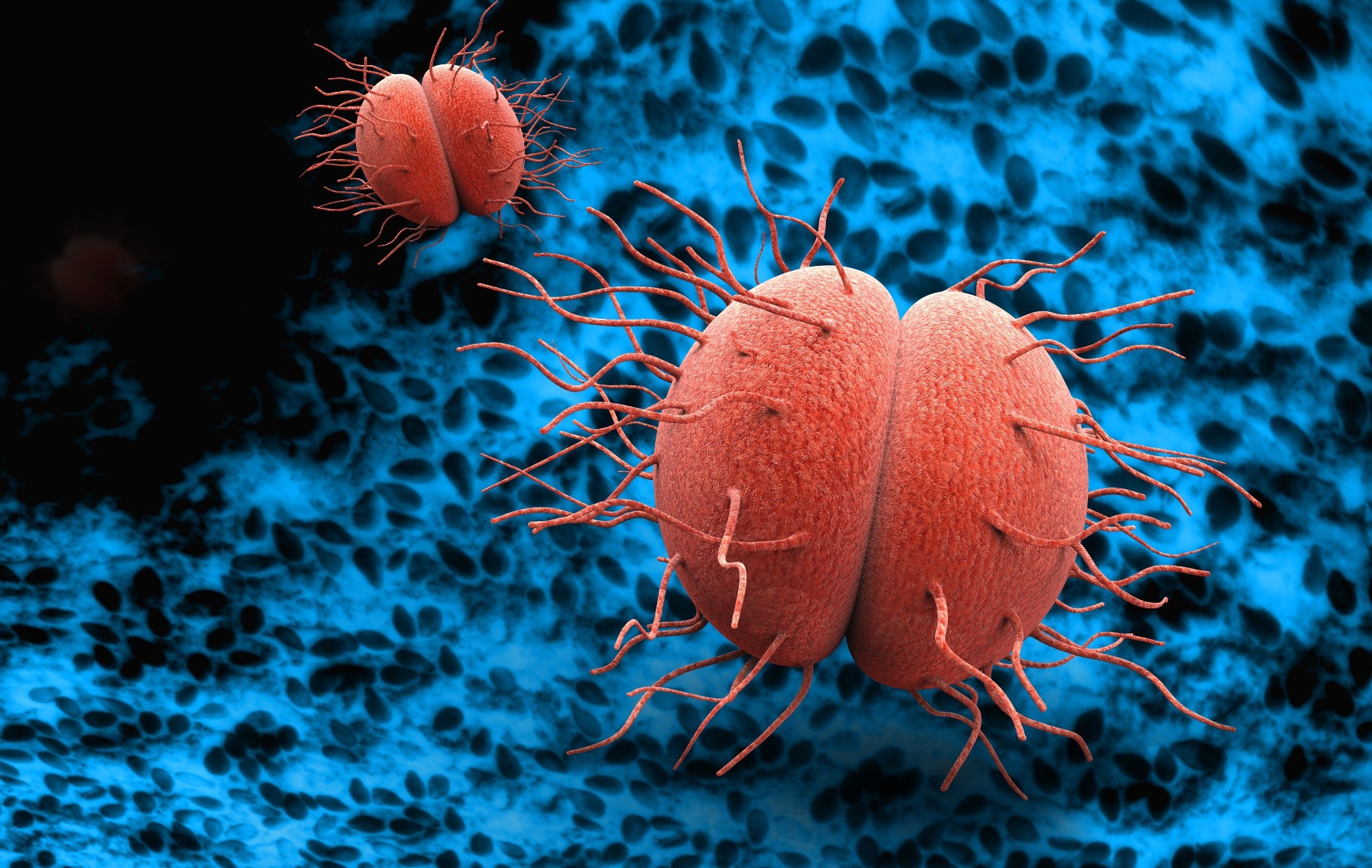 Study: Antimicrobial treatment and resistance in sexually transmitted bacterial infections. Image Credit: Giovanni Cancemi / Shutterstock
Study: Antimicrobial treatment and resistance in sexually transmitted bacterial infections. Image Credit: Giovanni Cancemi / Shutterstock
Background
STIs have affected humans for centuries, caused by diverse pathogens and manifesting in various syndromes. Despite medical advancements, the etiologies of some STI syndromes remain unexplained. These infections often lead to severe symptoms (including infertility and chronic pelvic pain), thereby causing significant global morbidity. Socioeconomic factors and behavioral trends influence STI prevalence. While antimicrobials offer treatment to an extent, concerns over AMR persist globally, particularly for N. gonorrhoeae and M. genitalium. Comprehensive approaches are needed to address these challenges effectively. To address this gap, researchers in the present review explore the epidemiology, treatment options, and the advent of AMR in various STIs while identifying key priorities to combat them.
Neisseria gonorrhoeae
Gonorrhoea remains prevalent globally, with an estimated 82 million cases annually, disproportionately affecting low- and middle-income countries (LMICs) and high-risk populations like sex workers and men who have sex with men (MSM). Incidence has surged in recent years, notably in high-income countries, posing significant public health challenges and risks of severe complications.
Antimicrobial treatment for gonorrhea focuses on empirical therapy. The combination of ceftriaxone and azithromycin is a common first-line option. However, rising resistance poses challenges, leading to considerations of monotherapy or alternative dual therapies. A better understanding of pharmacokinetics and pharmacodynamics of drug options is crucial for optimizing treatment efficacy and combating AMR in this disease.
N. gonorrhoeae has now developed resistance to all recommended antimicrobials, leaving ceftriaxone as the last effective option. Global surveillance programs like WHO GASP (World Health Organization Global Gonococcal Antimicrobial Surveillance Program) and Enhanced GASP monitor resistance trends, emphasizing the need for new treatments amid rising resistance. Whole-genome sequencing could help enhance our understanding of gonorrhea epidemiology and antimicrobial resistance transmission globally.
Mycoplasma genitalium
M. genitalium prevalence is estimated to be around 1.3% in high-income countries and 3.9% in LMICs, peaking in the age group of 20–30 years. It disproportionately affects MSM and sex workers, with detection challenges due to low bacterial load and variable test performances.
With limited antimicrobial options due to the lack of a bacterial cell wall, macrolides and fluoroquinolones have been preferred for these infections. However, increasing resistance to macrolides necessitates resistance-guided therapy, with moxifloxacin often used as a second-line treatment. Dual resistance to azithromycin and moxifloxacin presents a significant challenge, highlighting the urgent need for new treatment alternatives.
AMR in M. genitalium, primarily mediated by macrolide and fluoroquinolone resistance, poses a significant global concern. Resistance is attributed to single-nucleotide polymorphisms (SNPs), with resistance rates varying between regions and populations. Dual resistance to both macrolides and fluoroquinolones is escalating, highlighting the urgent need for new treatment options. The emergence of novel antimicrobials like zoliflodacin and gepotidacin presents promising alternatives, but challenges remain in addressing resistance effectively amid limited clinical data and evolving resistance mechanisms.
Chlamydia trachomatis
C. trachomatis, the most common bacterial STI, affects approximately 129 million individuals globally each year, with higher rates observed in sexually active individuals under 25 years of age. Most infections are asymptomatic, but when symptoms occur, they typically manifest as mucopurulent cervicitis, urethritis, conjunctivitis, or proctitis, with potential complications including pelvic inflammatory disease and infertility.
Treatment of this infection has remained straightforward, with no stable resistance to any antimicrobials demonstrated in clinical isolates. While both azithromycin and doxycycline are effective options, current recommendations lean towards 100 mg doxycycline twice daily for seven days due to its higher efficacy and lower risk of inducing resistance compared to the one-gram single-dose azithromycin regimen.
Treponema pallidum
Syphilis is a systemic infection and affects around 7.1 million individuals per year globally. Notable burdens have been observed among MSM and increasing cases in women and heterosexual men. Congenital syphilis rates have surged in some regions despite preventable mother-to-child transmission.
Penicillin, including benzathine penicillin G (BPG), remains the mainstay treatment for syphilis without reported resistance. Alternatives like procaine penicillin or doxycycline are available for penicillin-allergic patients, with azithromycin no longer recommended due to resistance.
Conclusion
In conclusion, the study calls for urgent action to address the lack of effective treatments for Neisseria gonorrhoeae and Mycoplasma genitalium infections due to AMR, particularly in low- and middle-income countries. Strengthening STI prevention (through counseling, screening, and condom use), monitoring post-exposure prophylaxis, developing vaccines, and improving point-of-care diagnostic and predictive tools are key priorities for reducing the burden of STIs. The prioritization of developing new antimicrobials, repurposing of older ones, and implementing holistic treatment strategies are essential to maintain the treatability of these STIs. Parallelly, addressing the stigma, shame, and discrimination associated with STIs is vital to ensure equitable access to healthcare services for all populations.