Atopic dermatitis, or eczema, is a common inflammatory skin ailment that may result from immunologic disturbance and dysfunction in the skin barrier, while its underlying pathophysiology remains unclear. Evidence suggests that vitamin D levels in early life may play a role in the development of eczema. Vitamin D deficiency and eczema prevalence are higher in regions with less sunlight. Vitamin D receptors in immune cells suggest its involvement in modulating immune responses. Evidence from cohort studies suggests a link between higher cord blood vitamin D levels and reduced risk of eczema in early childhood. However, clinical trials on women with vitamin D supplementation during gestation have yielded inconsistent results. Current guidelines do not universally recommend such supplementation due to limited evidence on its effects on allergic diseases in offspring.
Despite recognizing different eczema phenotypes, no studies have explored the association between longitudinal eczema development or phenotypes and neonatal vitamin D or 25(OH)D3, its most stable circulating form. Therefore, researchers in the present study aimed to explore how neonatal serum 25(OH)D3 levels relate to eczema prevalence at various ages between 1 and 25 and eczema phenotype up to age 25 years.
About the study
The Melbourne Atopy Cohort Study (MACS) followed 223 infants with a family history of allergic diseases, including self-reported asthma, allergic rhinitis, eczema, or severe food allergy, from birth to 25 years of age. The infants had Australian-born parents and high socioeconomic statuses. Data collection included telephone surveys, clinical examinations, and skin prick testing (SPT) at 6 months and 1, 2, 12, 18, and 25 years. At age 18, participants consented to access their newborn screening cards for measuring neonatal 25(OH)D3 levels via dried blood spots (DBS).
Prevalent eczema was defined based on parental or self-reports of eczema diagnosis or rash treated with topical steroids. Longitudinal eczema phenotypes were identified using latent class analysis, resulting in the following subclasses: early-onset-resolving eczema, early-onset persistent eczema, mid-onset-resolving eczema, mid-onset persistent eczema, and minimal/no eczema. Eczema/sensitization phenotypes were determined based on eczema and allergen (cow's milk, egg white, peanut, house dust mite, cat dander, and ryegrass) sensitization, with participants categorized into atopic eczema, non-atopic eczema, asymptomatic-sensitized, or asymptomatic groups at each age.
Statistical analysis involved using logistic regression models, odds ratios, generalized estimation equations (GEEs), likelihood ratio tests, Wald tests, directed acyclic graphs, and sensitivity analysis.
Results and discussion
The peak prevalence of eczema was found to be in infancy (31.2%), declining to 15.9% at age 6 years and rising to 26% at age 25. The median sera-adjusted level of 25(OH)D3 for the DBS samples was found to be 32.5 nmol/L. Consistent with expectations, a significant association was observed between vitamin D levels and the birth season (p < 0.001), indicating that children born in winter had lower 25(OH)D3 levels. In the sensitivity analysis, adjusting for birth season, higher neonatal vitamin D levels were associated with reduced eczema risk at 1–2 years. Maternal smoking during pregnancy was found to modify the association. Further, higher neonatal vitamin D level was found to be associated with a reduced eczema risk at age 2 years in participants with maternal smoking history, as compared to those without it.
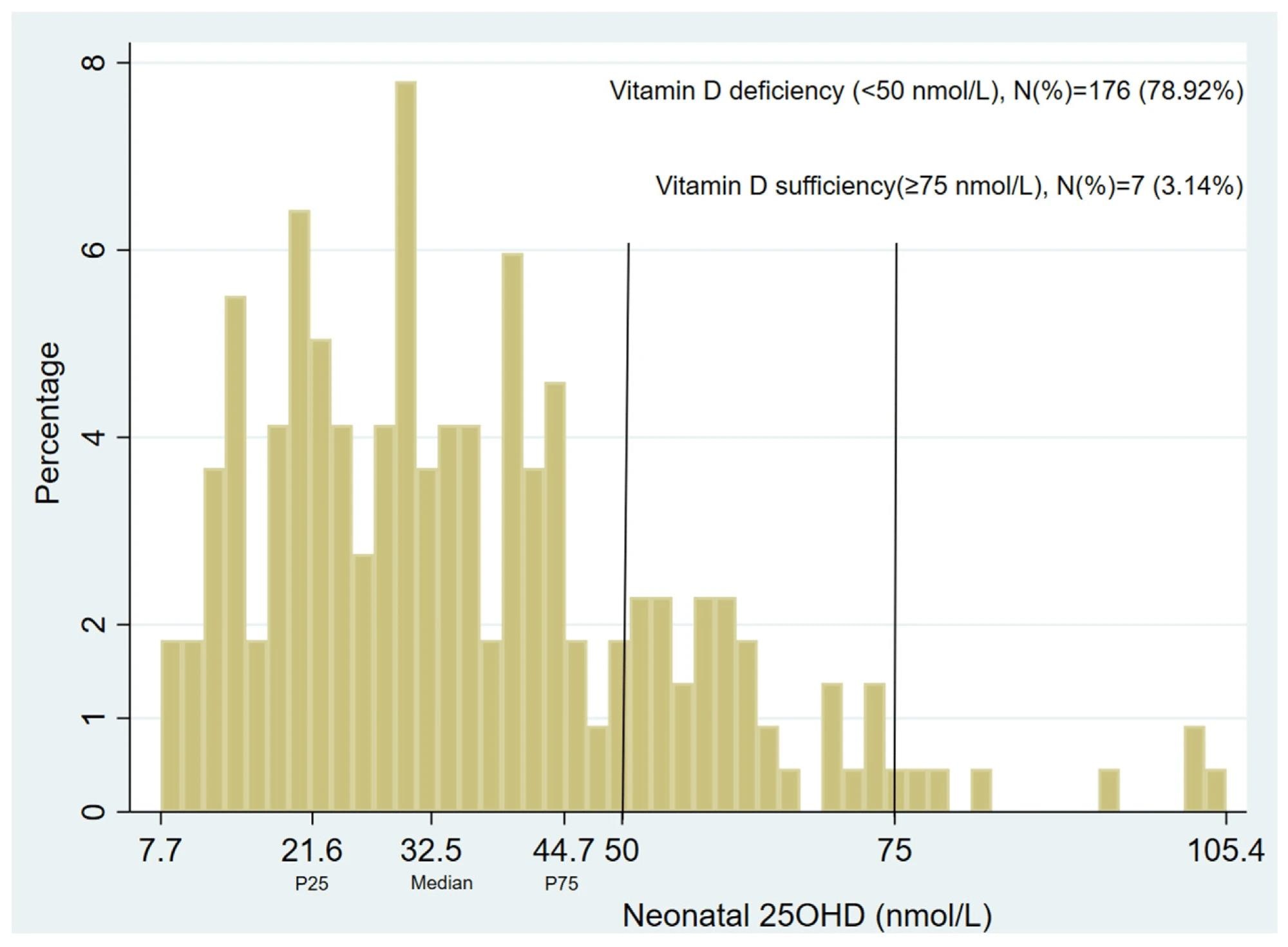 The neonatal vitamin D (25(OH)D3) level in 223 MACS participants. The median level was 32.5 nmol/L. P25 was 21.6 nmol/L, P75 was 44.7 nmol/L, and mean was 35.9 ± 18.6 nmol/L.
The neonatal vitamin D (25(OH)D3) level in 223 MACS participants. The median level was 32.5 nmol/L. P25 was 21.6 nmol/L, P75 was 44.7 nmol/L, and mean was 35.9 ± 18.6 nmol/L.
Higher neonatal vitamin D levels were found to be linked to a decrease in the risk of early-onset persistent eczema (aMOR = 0.74), as well as an increase in the risk of early-onset-resolving eczema (aMOR = 1.30) compared to minimal/no eczema subclass up to age 12 years. Similar trends persisted for eczema phenotypes for up to 25 years. Mother's birthplace influenced the association— elevated neonatal vitamin D levels were linked to reduced odds of early-onset persistent eczema up to 12 years in children with non-Australian/New Zealand-born mothers but not for those with Australian/New Zealand-born mothers. Paternal education and maternal prenatal smoking were also found to modify the association with eczema phenotypes up to 25 years.
The study is strengthened by its control for various confounding factors and prospective design. However, the study is limited by its small sample size, attrition over time, potential for reduced precision in estimates, and low generalizability beyond high-allergy-risk cohorts.
Conclusion
In conclusion, the study indicates that elevated neonatal vitamin D levels could potentially lower the likelihood of early-onset persistent eczema, subject to potential modifications by maternal smoking during pregnancy and birthplace. Further observational studies in diverse populations are necessary to validate these findings. Additionally, well-designed clinical trials are warranted to explore the effectiveness of maternal vitamin D supplementation in preventing eczema, particularly early-onset persistent cases.
Journal reference:
- Neonatal Vitamin D and Associations with Longitudinal Changes of Eczema up to 25 Years of Age. Zeng R. et al., Nutrients, 16(9):1303 (2024), DOI: 10.3390/nu16091303, https://www.mdpi.com/2072-6643/16/9/1303