In a recent study published in the journal Cell, a team of researchers investigated the association between intestinal Blastocystis (a single-celled organism found in the human gut, linked to health outcomes with at least 28 subtypes (STs)), diet, and cardiometabolic health, highlighting its potential beneficial role in personalized responses to diet and disease outcomes.
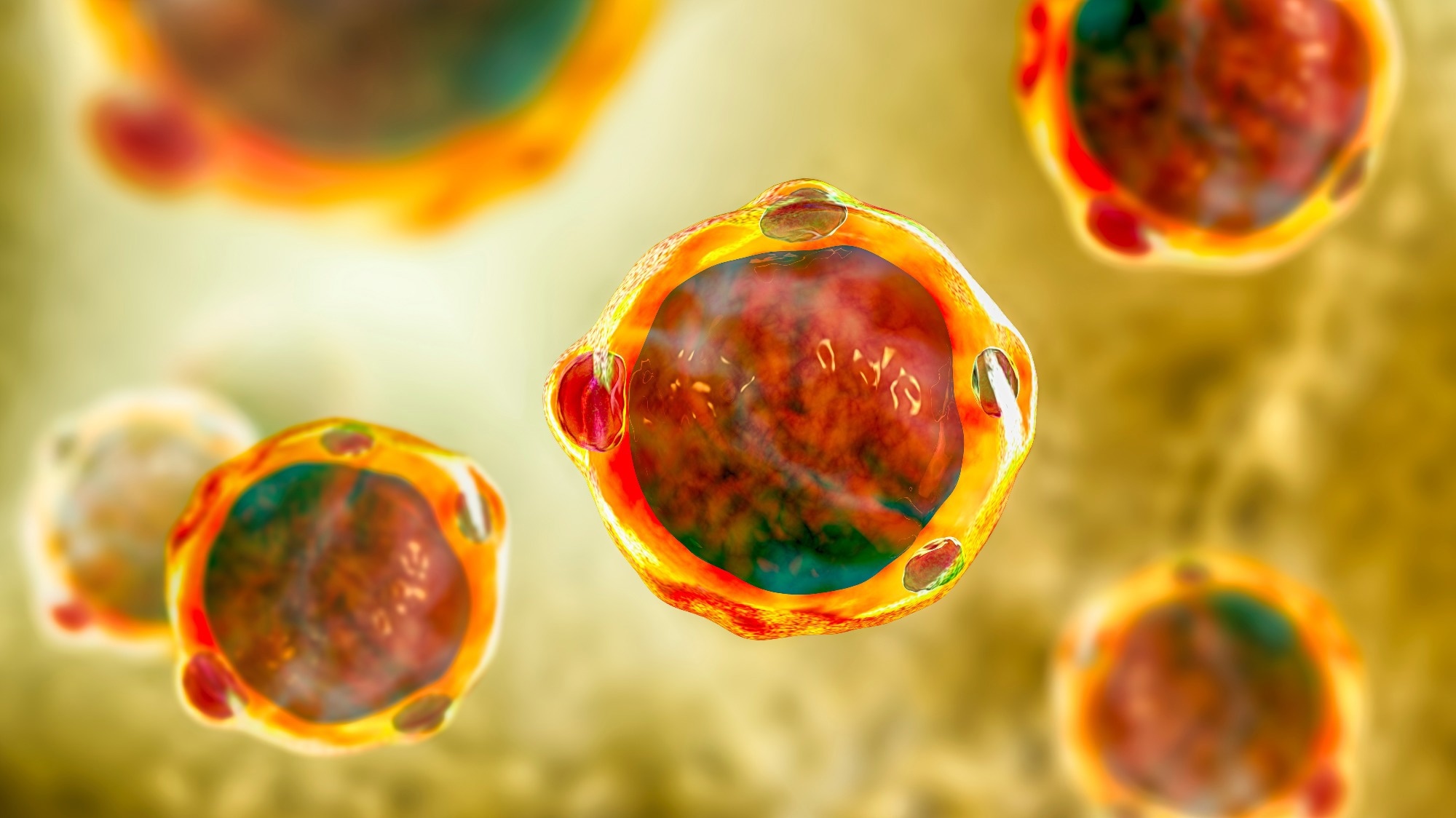 Study: Intestinal Blastocystis is linked to healthier diets and more favorable cardiometabolic outcomes in 56,989 individuals from 32 countries. Image Credit: Kateryna Kon / Shutterstock
Study: Intestinal Blastocystis is linked to healthier diets and more favorable cardiometabolic outcomes in 56,989 individuals from 32 countries. Image Credit: Kateryna Kon / Shutterstock
Background
Decades of evidence link dietary intake with chronic disease development. High-quality diets are generally endorsed to reduce long-term disease risk, though benefits vary individually. A single cohort study found that gut microbial communities with Blastocystis are associated with improved glucose responses, body adiposity, and other biomarkers. ST1, ST2, and ST3 are the most common in humans. Further research with more extensive, diverse cohorts and detailed dietary data is needed to understand the relationship between gut Blastocystis, nutrition, and cardiometabolic health. This will help clarify how Blastocystis influences host health and its role in personalized nutrition and disease prevention.
About the study
To characterize the presence of Blastocystis at the global level, the study identified and collected data from 61 publicly available cohorts with shotgun metagenomic samples of the human gut microbiome from curatedMetagenomicData version 3 (cMD3). The datasets included information on host age, sex, country of origin, and body mass index (BMI), resulting in a total of 73 datasets and stool metagenomes from 56,989 distinct individuals. Among these, 41,428 were from healthy/control individuals, and 15,561 were considered "unhealthy." Additionally, 1,034 individuals had available longitudinal gut microbiome samples.
The study also included 1,124 healthy individuals from the Personalized REsponses to DIetary Composition Trial (ZOE PREDICT) personalized diet intervention study, with microbiome samples collected before and after the intervention. Samples from other human body sites, including the oral cavity and skin, as well as 28 ancient human metagenomes from paleofeces, were included. The non-human dataset comprised 4,590 gut metagenomes from 214 species across various animal taxa. All samples were profiled using a validated computational workflow to determine the presence and abundance of eight genetically distinct Blastocystis STs previously described in humans. The global Blastocystis prevalence was found to be highly variable and confined to gut microbial communities.
Study results
The analysis included 56,989 human gut microbiome samples from 73 datasets, with comprehensive information on host demographics and health status. The ZOE PREDICT studies provided detailed dietary and health data, revealing that Blastocystis prevalence and ST distribution varied widely by geography, age, and lifestyle.
Participants with higher diet quality were more likely to carry Blastocystis, which was associated with favorable cardiometabolic markers, such as lower BMI, improved glucose tolerance, and healthier lipid profiles. This association was validated across multiple cohorts, showing a consistent negative relationship between Blastocystis presence and body adiposity and reduced prevalence of disorders linked to gut microbiome disturbances, including inflammatory bowel diseases, colorectal cancer, and diabetes.
In a personalized diet intervention study involving 1,124 participants, improvements in diet quality correlated with increased Blastocystis prevalence and abundance, further supporting the beneficial role of Blastocystis in human health. The findings suggest that Blastocystis might serve as a marker for a healthier lifestyle and could play a beneficial role in personalized responses to diet and disease susceptibility.
The study also explored the relationships of Blastocystis ST carriage with geographic and lifestyle differences, finding that ST1 and ST2 were more prevalent in non-Westernized populations. At the same time, ST4 was detected primarily in Westernized individuals. The persistence of Blastocystis colonization was evaluated through longitudinal sampling, showing that individuals typically remained positive or negative over time, with the same ST maintained in most cases. Subgroup analyses among monozygotic and dizygotic twins indicated that Blastocystis carriage is likely influenced more by environmental factors than host genetics.
Diet significantly impacted Blastocystis prevalence, with higher consumption of unprocessed plant-based foods linked to higher Blastocystis carriage. Conversely, Blastocystis-negative individuals consumed more processed and less healthy foods. Improved diet quality in the ZOE PREDICT studies was associated with higher Blastocystis prevalence and abundance, supporting its potential role in enhancing cardiometabolic health.
Meta-analyses confirmed the association between Blastocystis and lower BMI and its enrichment in healthy controls compared to individuals with various chronic diseases.
Conclusions
To summarize, the study profiled Blastocystis from 56,989 human microbiome samples, finding it prevalent worldwide with variability by geography, lifestyle, and diet. ST4 was common in Westernized regions but rare in Asia and absent in South America and Africa. Blastocystis was linked to healthier diets and favorable cardiometabolic profiles, with higher prevalence in those consuming plant-based, minimally processed foods. A longitudinal study showed that improved diet quality increased Blastocystis prevalence. The analysis found lower BMI and better glycemic and lipid profiles in Blastocystis-positive individuals. These findings suggest Blastocystis may be a beneficial component of the gut microbiome, challenging its pathogenic perception.